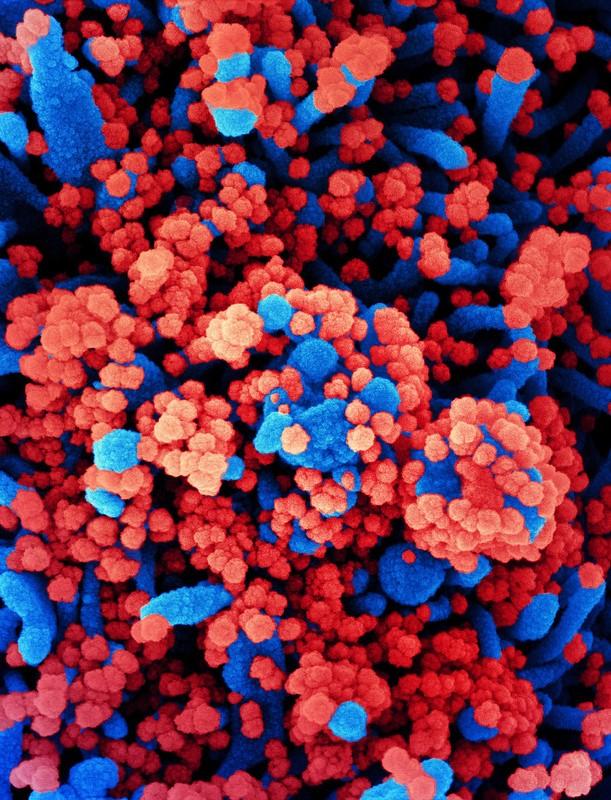
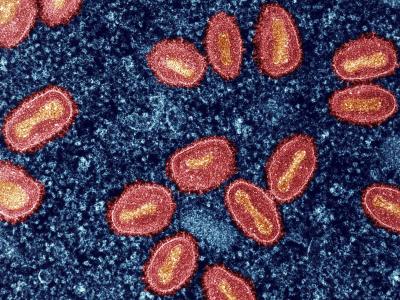
People who had COVID-19 had an 84% lower risk of becoming reinfected and a 93% lower risk of symptomatic infection during 7 months of follow-up, according to findings from a large, multicenter study published late last week in The Lancet.
The prospective cohort SARS-CoV-2 Immunity and Reinfection Evaluation (SIREN) study, by Public Health England Colindale researchers, involved 25,661 workers at public hospitals throughout England who were tested for SARS-CoV-2 every 2 to 4 weeks and antibodies at enrollment and every 4 weeks. Volunteers also completed questionnaires on symptoms and exposures every 2 weeks.
Of the 25,661 participants, 32.3% were assigned to the baseline positive (possibly or probably previously infected) group, and 67.7% were assigned to the negative group. Of the 8,278 positive participants, 91.2% had SARS-CoV-2 antibodies at study enrollment, while 7.0% were negative for antibodies but had a previously positive antibody and/or coronavirus test, and 1.8% had tested positive for COVID-19 but didn't have linked antibody data.
Far fewer symptomatic infections
From June 2020 to January 2021, 1.4% of the 8,278 participants who previously had COVID-19 were infected, compared with 9.8% of 17,383 initially coronavirus-naïve participants. Infections in the baseline-positive group peaked in the first week of April, while they peaked in the negative group the last week of December.
Incidence density was 7.6 new infections per 100,000 person-days in those previously infected, versus 57.3 per 100,000 person-days in those without previous infection. Compared with primary infections, the adjusted incidence rate ratio was 0.16 for reinfections. Median time between primary infection and reinfection was more than 200 days.
Among the baseline-positive group, 50.3% of infections were symptomatic, with 32.3% involving usual coronavirus symptoms. Among the baseline-negative cohort, 80.3% of infections were symptomatic, 66.1% of them involving usual COVID-19 symptoms.
The authors noted that, late in the follow-up period, from Dec 8, 2020, to Jan 11, 2021, 52.2% of all participants were vaccinated against SARS-CoV-2. Thus, 0.4% of the study's person-time follow-up included participants 21 or more days after vaccination, which the researchers said likely had only a modest effect on the results.
Median participant age in the baseline-positive cohort was 45.7 years, 84.2% were women, and 87.3% were White. Median follow-up was 275 days in the positive group and 195 days in the negative group.
"This study shows that previous infection with SARS-CoV-2 induces effective immunity to future infections in most individuals," the authors wrote. "The importance of understanding the nature and rate of SARS-CoV-2 reinfection to guide non-pharmaceutical interventions and public health control measures is essential in this evolving pandemic."
Natural immunity vs vaccine protection
In a commentary in the same journal, Florian Krammer, PhD, of the Icahn School of Medicine at Mount Sinai in New York City, said that although natural infection tends to induce lower and more variable antibody concentrations than COVID-19 vaccines, "the findings of the authors suggest that infection and the development of an antibody response provides protection similar to or even better than currently used SARS-CoV-2 vaccines.
He added, "The SIREN study adds to a growing number of studies, which demonstrate that infection does protect against reinfection, and probably in an antibody-dependent manner."
Krammer pointed out that the researchers didn't link quantitative antibody measurements to protection against infection afforded by natural infection versus vaccines, a topic that should be a priority for future studies.
"Establishment of antibody titres as a correlate of protection and defining a protective titre would be extremely important for public health considerations and for patient management," he wrote. "A correlate of protection and a protective threshold would also allow for the development of additional SARS-CoV-2 vaccines based on small immunogenicity-based phase 3 trials rather than large and costly field efficacy trials, which are becoming exceedingly difficult to perform."