New research by a team of scientists in Israel indicates that when bacteria develop tolerance to an antibiotic, adding a second antibiotic to the treatment regimen may not work out as intended.
In a paper published last week in Science, researchers from The Hebrew University and Shaare Zedek Medical Center in Jerusalem set out to determine whether the development of antibiotic tolerance occurs in people and affects treatment. The emergence of tolerance mutations in response to antibiotics, as the researchers had previously observed in lab experiments, allows bacteria to survive limited antibiotic treatment and can subsequently promote the evolution of resistance.
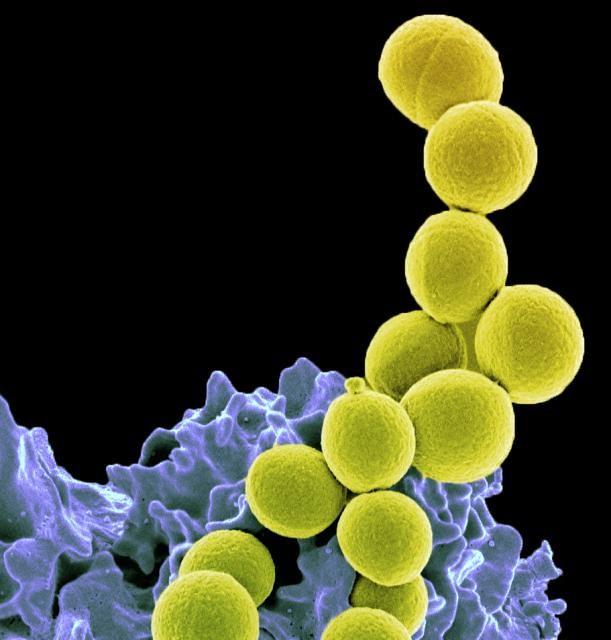
To see whether this pattern occurs in human infections, the researchers examined isolates from two patients at Shaare Zedek Medical Center who'd been treated for methicillin-resistant Staphylococcus aureus (MRSA) bacteremia. Despite treatment with a combination of antibiotics, the infections had lasted for 2 weeks.
Surprise findings
What they found surprised them. One of the patients was originally treated with vancomycin, and tolerant strains developed within 4 days, at which point rifampicin was added to the treatment regimen. When the infection was still present on day 8, vancomycin was replaced with daptomycin. Adding rifampicin to daptomycin has been shown in previous studies to be an effective strategy for complex MRSA infections, with rifampicin countering resistance to daptomycin.
But in this case, the researchers observed that the combination wasn't effective. Further analysis showed that the isolates that had developed tolerance to vancomycin had also developed tolerance to daptomycin, and in these isolates, lab experiments showed that resistance to rifampicin quickly emerged after it was added to the regimen. In contrast, no resistance to rifampicin was observed when the drug was tested in isolates collected on day 1 of treatment, before tolerance to vancomycin or daptomycin had emerged.
"Our analysis of strains isolated from blood infections revealed a notable similarity to in vitro experiments. In both, the rapid evolution of tolerance was identified as a major survival factor, followed by the emergence of resistance," the authors of the study write. "However, in contrast to the in vitro evolution results (where a single drug was used), our study shows how tolerance promotes the evolution of resistance under combination treatments that are expected to prevent resistance."
And the results don't apply just to Staphylococcal bacteria. When the researchers measured bacterial growth in Escherichia coli in response to drug combinations from four different antibiotic classes, they found that isolates with tolerance to norfloxacin and ampicillin promoted resistance in some of the combinations.
"We conclude that rescue of resistance mutations by tolerance is a general phenomenon that may have crucial implications for the evolution of resistance in patients treated with combinations of antimicrobials," they add.
Better diagnostics needed
In an accompanying commentary on the study, clinical pharmacists from Wayne State University and the University of Minnesota say the finding that this phenomenon applies to gram-negative bacteria and other antibiotic-combination therapies has profound implications, since clinical labs lack methods for screening for antibiotic tolerance.
They say the development and implementation of more rapid diagnostics for antibiotic tolerance will be necessary to help clinicians determine whether combination therapy is warranted.
"Although these results suggest that many benefits of combination therapy are lost when microbes become tolerant, additional studies assessing clinical outcomes in patients with antimicrobial-tolerant infections will be necessary to guide clinical decisionmaking," they write. "In the meantime, when choosing combination antibiotic therapies, perhaps ensuring adherence to a zero-tolerance policy is best."
See also:
Jan 10 Science study
Jan 10 Science commentary