Fungal diseases may not get as much attention as bacterial or viral infections, but they affect millions of people. And as resistance to current antifungal treatments emerges, the problem is likely to get worse.
Globally, there are an estimated 1 million cases of cryptococcal meningitis per year. Invasive candidiasis and pneumocystis pneumonia each affect more than 400,000 annually and aspergillosis more than 200,000. These are just the leading invasive fungal infections. The infections frequently occur in patients with severely weakened immune systems such as HIV, cancer, and organ transplant patients and they are often deadly, with some carrying mortality rates as high as 95%. Yet the general public hears little about them.
"These infections cause tremendous morbidity and mortality around the world, and they have flown under the radar for so long," infectious disease expert and pharmaceutical executive Oren Cohen, MD, told CIDRAP News.
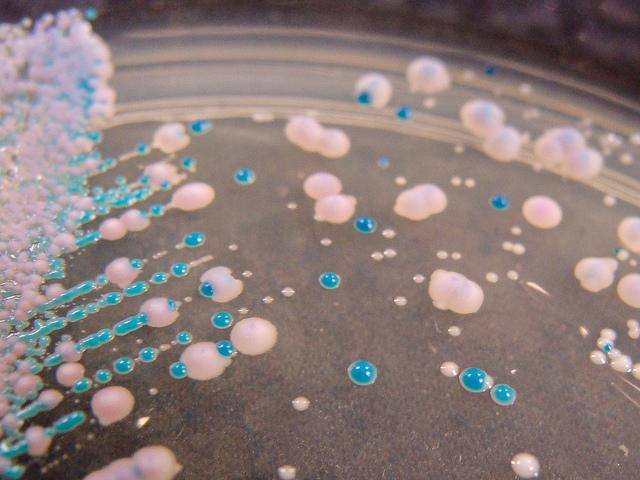
But that may be changing. In the past year, officials with the Centers for Disease Control and Prevention (CDC) have been keeping their eye on a small but steady rise in deadly invasive infections caused by Candida auris, a new member of the Candida family that has shown growing resistance to three of the classes of drugs used to treat invasive fungal infections—azoles, echinocandins, and polyenes—and appears to be capable of spreading from patient to patient. C auris is one of the invasive fungal diseases that's been highlighted this week during the CDC's first-ever Fungal Disease Awareness Week.
"Candida auris is clearly making a case for the fact that highly resistant fungi are out there, they can be deadly, and it can be a rapidly spreading problem," Cohen said.
New treatment options are needed
The emergence of multidrug-resistant C auris highlights another aspect of fungal infections that has garnered little public attention: Like many species of pathogenic bacteria, pathogenic fungi are growing resistant to the drugs used to treat them. In the oldest antifungals (polyenes) and the newest (echinocandins), emerging resistance is making it more difficult to treat patients with invasive fungal infections.
Cohen, chief medical officer of Viamet Pharmaceuticals, is hoping his company might be able to provide a solution to this problem. In preclinical studies conducted in collaboration with the CDC, Viamet's novel oral agent VT-1598 demonstrated robust activity against 100 clinical isolates of C auris, including those with known resistance to other antifungals. The drug has also shown broad-spectrum activity against other Candida species, members of the Aspergillus family, Cryptococcus species, and coccidioidomycosis, also known as valley fever.
"I think this has the potential to really alter the treatment paradigm for a number of invasive fungal infections," Cohen said.
Further along is SCY-078, an oral and intravenous agent from biotechnology company Scynexis that's in phase 2 clinical development for invasive infections caused by Candida and Aspergillus species. In a study in Antimicrobial Agents and Chemotherapy, SCY-078 also showed potent activity against drug-resistant clinical C auris isolates, and phase 2 studies indicate a good safety and tolerability profile.
"We're confident this product could be used and will be helpful for patients who will get these very serious infections," Marco Taglietti, MD, president and chief executive officer of Scynexis, said in an interview.
These novel drugs, and other new antifungal agents in development, will be a significant addition to what is a limited set of options for physicians treating patients with invasive fungal infections. "This is what the medical community is really waiting for—new classes of antifungals," he said.
While emerging resistance to treatment is an issue for both antibiotics and antifungals, said Taglietti, it's a bigger problem with antifungals because there are only the three major structural classes plus a handful of drugs with antifungal properties, such as flucytosine. Resistance is further narrowing those treatment options. And since fungal infections can be very aggressive and need to be treated quickly, he explained, resistance will continue to grow as physicians are forced to keep going back to their only options.
"You don't have time to really try something that may not be that effective, because you may lose your patient," Taglietti said.
Toxicity and tolerability
On top of the resistance issue, use of some currently available antifungal drugs is limited by high toxicity. For example, take the current "gold-standard" treatment for cryptococcal meningitis, a regimen of amphotericin B and 5-flucytosine, which has been used for more than 50 years. "That's such miserable therapy," Cohen said, adding that amphotericin is associated with fevers, chills, renal toxicity, and blood toxicity. "It is the most effective…but the tolerability is absolutely horrible."
That tolerability is likely one of the reasons why there is still high mortality in cryptococcal meningitis patients who receive treatment, Cohen explained, because clinicians frequently have to reduce or even skip doses. Toxicity is a problem with antifungals because fungi and humans are both eukaryotes, and drugs that target genes in fungi can also attack homologous genes in human cells.
Both Taglietti and Cohen said there are many challenges to developing new antifungal drugs and bringing them to market. These agents must either kill fungus or effectively control fungal growth as well as attack specific targets in fungi without also harming human tissue and organs. Ideally, they should be effective against a broad spectrum of fungal pathogens. So far, finding that magic combination has proved difficult. In addition, there are many of the same financial and regulatory hurdles that have hampered new antibiotic development. But both men are optimistic about the future of antifungal development.
"The good news is that there are now several companies trying to bring new products to the market, innovative products," Taglietti said. "So I'm confident that we will be able, in the next few years, to improve the armamentarium of doctors."
See also:
Aug 9 CDC press release
Jun 5 Viamet press release
May 11 Scynexis press release