Jun 7, 2012 (CIDRAP News) – Two groups of tuberculosis (TB) researchers released new findings today, giving the world its first look at drug-resistant TB at the national level in China and presenting encouraging findings for the new antibiotic delamanid for the multidrug-resistant (MDR) form of the disease.
Both studies were published today in an early online edition of the New England Journal of Medicine (NEJM), along with an accompanying editorial.
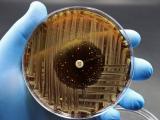
One study, a survey of drug-resistant TB in China, was conducted in 2007 by the Chinese Center for Disease Control and Prevention. Previously, experts have based their estimates of disease burden in China on local and regional findings. The current investigators used cluster-randomized sampling of TB patients seen mainly in clinic settings, testing them for resistance to first-line and second-line TB drugs.
Of 3,037 patients with new TB infections and 892 who were previously treated, 5.7% and 26.7%, respectively, had MDR-TB. Among these patients, 8% had extensively drug-resistant (XDR) TB. Most MDR-TB and XDR-TB cases involved primary transmission, with the highest MDR-TB risk in those who had received their last treatment in a TB hospital.
When the researchers looked at previously treated MDR-TB patients, they found that 43.8% had not completed their last treatment. Among those who had completed their treatment regimen, 90.6% experienced relapsed TB, and most of those (61.7%) had been treated in the clinic setting.
The authors wrote that the findings confirm that China has a serious drug-resistant TB problem, and that, based on World Health Organization (WHO) MDR-TB estimates, China has the highest annual number of MDR-TB cases each year in the world.
The situation could easily be worse, they wrote, noting that 11% of new drug-resistant TB patients and 16% of previously treated drug-resistant TB patients are just one step away from having MDR-TB, and more than a third of MDR-TB patients are one step away from having XDR-TB.
The researchers said the findings point to a need for more interventions to prevent MDR-TB in China, such as resistance testing at local clinics before treatment is started, improved treatment in hospitals, and better systems for definitive diagnosis.
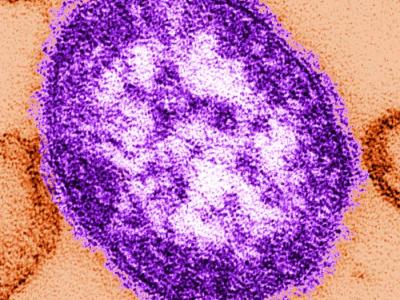
In the second study, researchers reported findings from a randomized, placebo-controlled, multinational trial of the new tuberculosis medication delamanid, a mycolic acid synthesis inhibitor that has shown in vitro and in vivo activity against drug-resistant strains of Mycobacterium tuberculosis.
The study, conducted at 17 centers in nine countries, was designed to test the safety and efficacy of two dosages of the drug. Study patients were adults with culture-confirmed MDR-TB and chest films consistent with TB. They were hospitalized during the 8-week treatment period and were monitored for an additional 4 weeks. In addition to a background drug regimen developed according to WHO guidelines, patients received either 100 mg or 200 mg of delamanid or placebo twice a day. Sputum samples were obtained 14 times over the intervention and follow-up periods.
Of patients who received the 100-mg dose of the drug, 45.4% had sputum-culture conversion (defined as five successive weekly cultures negative for M tuberculosis) at 2 months, compared with 29.6% of those on the placebo regimen (P=0.008). The corresponding percentage of conversion among patients receiving the 200-mg dose of delamanid was 41.9% (P=0.04).
The investigators found that adverse events were mild to moderate and were spread evenly across the different groups. QT-interval prolongation was reported significantly more often in the patients who were receiving delamanid, but no clinical events were reported.
The authors said that further studies are under way to assess both the duration of efficacy and how safe the drug is when taken for longer periods, as well as a large trial to gauge 6 months of delamanid treatment that includes some patients with HIV co-infections.
In an editorial in the same issue of NEJM addressing both studies, two researchers from Johns Hopkins University called for increased screening and more rapid testing of the estimated 9 million people in the world with TB. Richard Chiasson, MD, and Eric Nuermberger, MD, wrote in the editorial that the rising spread of drug-resistant TB poses an "enormous challenge" to eradicating the disease, which is fatal in about 1.5 million people each year and exacts the highest burden in developing countries. Chiasson is professor of medicine at Johns Hopkins School of Medicine and founding director of its Center for Tuberculosis Research, and Nuermberger is associate professor of medicine in the infectious diseases division.
They noted that a worrisome finding of the Chinese survey study is that the majority of the drug-resistant cases occurred in people with newly diagnosed TB rather than in people who didn't respond to therapy or relapsed after treatment, which suggests person-to-person spread of drug-resistant organisms.
Chiasson said that the large-scale resistance seen among new TB cases strengthens the case for not limiting drug-resistance testing to previously treated patients, according to a Jun 6 EurekAlert press release. He also noted that same-day testing is more expensive than current methods—$40 per person compared with $5, but said the added cost is worthwhile, given what they call the sobering scope of the problem.
In addressing the drug study, the two editorialists wrote that new antibiotics are the key to controlling TB in all its drug-resistant forms. Though the results for delamanid are encouraging, the drug is but "half the answer."
Nuermberger said in the press release that the delamanid findings are similar to 2009 findings for another new antibiotic, bedaquiline, which eradicated TB in sputum in 48% of study participants. He added that new antibiotics are good news but said what TB healthcare providers need most is better information about what drug combinations work best and guidelines about using new antibiotics.
The two authors urged regulators, pharmaceutical companies, and researchers to speed efforts to evaluate the impact of the new drugs in different combinations.
Zhao Y, Xu S, Wang L, et al. National survey of drug-resistant tuberculosis in China. N Engl J Med 2012 Jun 7;366(23):2161-70 [Abstract]
Gler MT, Skripconoka V, Sanchez-Garavito E, et al. Delamanid for multidrug-resistant pulmonary tuberculosis. N Engl J Med 2012 Jun 7:366(23):2151-60 [Abstract]
Chiasson RE, Nuermberger EL. Confronting multidrug-resistant tuberculosis. (Editorial) N Engl J Med 2012 Jun 7;366(23):2223-4 [Extract]
See also:
Jun 6 EurekAlert press release