A new study in the Journal of the Pediatric Infectious Diseases Society describes what is believed to be the first case of bacterial meningitis caused by beta-lactamase–producing, ciprofloxacin-resistant Neisseria meningitidis in the United States.
The case occurred this January in a previously healthy 5-month-old Maryland boy who was treated in the emergency department at Children's National Hospital in Washington, DC. Although the boy was treated with broad-spectrum antibiotics and released after 7 days in the hospital, susceptibility testing of bacterial samples from the boy revealed resistance to five antibiotics—including penicillin and ciprofloxacin, which are typically used for treatment of people with confirmed N meningitidis infections and for prevention in those who've been in close contact with infected patients.
The authors of the study say the finding suggests that routine susceptibility testing of meningococcal isolates could help guide treatment and prophylaxis.
Not a typical case of bacterial meningitis
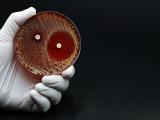
N meningitidis is the leading cause of bacterial meningitis, a sudden-onset, life-threatening infection of the lining of the brain and spinal cord or the bloodstream. Clinicians typically treat bacterial meningitis empirically with the broad-spectrum antibiotic ceftriaxone while they await blood culture results and cerebrospinal fluid tests to determine the causative pathogen. Early diagnosis and antibiotic treatment is critical.
That's the protocol that clinicians at Children's National Hospital followed with the 5-month-old boy, who came to the emergency department after 6 days of fever and congestion and increasing irritability. The boy was treated with ceftriaxone, and blood culture results and polymerase chain reaction (PCR) testing confirmed the infection was caused by N meningitidis.
In a typical case of bacterial meningitis, antibiotic therapy would have been switched at this point to penicillin or ampicillin, which have a narrower spectrum of activity. And antibiotic susceptibility testing isn't normally conducted on N meningitidis because the bacterium has historically been susceptible to these antibiotics.
But as report co-author and treating physician Gillian Taormina, DO, explains, the hospital's microbiology lab director, Joseph Campos, PhD, prefers to run beta-lactamase tests on N meningitidis because of increasing resistance that's been observed in other Neisseria bacteria in recent years. Beta-lactamases are enzymes that help bacteria overcome penicillin and other beta-lactam antibiotics. Surprisingly, the rapid test used by Campos identified a beta-lactamase in the isolate.
"This is very unusual for Neisseria meningitidis," Taormina said. "There have been a couple of cases in other countries over the last few decades that had a beta-lactamase–producing Neisseria meningitidis, but this was the first time that we could find in the literature that this has happened in the United States."
Taormina says it's unclear whether the boy wouldn't have responded to penicillin, since in vitro resistance doesn't always translate into in vivo resistance, but because of the test results, they decided not to take that risk and stuck with ceftriaxone.
Because of the surprise finding, Taormina and her colleagues sent the isolates on to the Maryland Department of Health (MDH) and the Centers for Disease Control and Prevention (CDC). Additional CDC testing confirmed the resistance to penicillin and also found resistance to ampicillin, trimethoprim-sulfamethoxazole, ciprofloxacin, and levofloxacin. Whole-genome sequencing (WGS) identified the beta-lactamase gene as blaROB1 and also identified a genetic mutation conferring resistance to ciprofloxacin.
That finding led Taormina and her colleagues to recommend rifampin instead of ciprofloxacin to the six family members who needed post-exposure prophylaxis.
Surveillance identifies additional resistant isolates
The hospital's decision to share this information with MDH and the CDC led to a larger study by the two agencies that identified 33 beta-lactamase–producing N meningitidis isolates from 12 states, 11 of which were also ciprofloxacin resistant. That study was published Jun 18 in the CDC's Morbidity and Mortality Weekly Report.
"These findings show that penicillin-resistant and ciprofloxacin-resistant meningococci are now present in the United States; however, the complete geographic and temporal distribution of these resistant meningococci is unclear, because not all U.S. meningococcal disease cases have isolates available for WGS or antimicrobial susceptibility testing," the authors wrote.
The study was accompanied by a CDC health advisory urging healthcare providers to test meningococcal isolates for susceptibility to penicillin. The advisory also asked state health departments to report any suspected meningococcal treatment of prophylaxis failures.
Taormina said collecting and testing more N meningitidis isolates will be necessary to see if resistance to penicillin and ciprofloxacin is more widespread. And if it is, she thinks routine beta-lactamase and susceptibility testing of N meningitidis isolates should be considered.
"If we do find this to be a widespread problem, as we think it might be, I think standards of practice might change, and people might be doing this testing more routinely," she said.