 A review and meta-analysis of randomized controlled studies (RCTs) found that short-course antibiotic therapy for ventilator-associated pneumonia (VAP) did not result in increased recurrence or relapse, French researchers reported yesterday in eClinical Medicine.
A review and meta-analysis of randomized controlled studies (RCTs) found that short-course antibiotic therapy for ventilator-associated pneumonia (VAP) did not result in increased recurrence or relapse, French researchers reported yesterday in eClinical Medicine.
The review identified five relevant studies comparing treatment for VAP with short-course (8 days or less) versus long-course (10 to 15 days) antibiotic therapy. Despite guidelines for VAP treatment, the optimal antibiotic duration remains unclear, especially for VAP caused by non-fermenting gram-negative bacteria (NF-GNB).
The primary end point for the meta-analysis was recurrence and relapse of VAP. Secondary end points included 28-day mortality, mechanical ventilation duration, number of extra-pulmonary infections, acquisition of multidrug-resistant (MDR) pathogens, and length of intensive care unit (ICU) stay.
The five studies included 1,069 patients, with 530 in the short-course group and 539 in the long-course group. There was no significant difference between short-course therapy (odds ratio [OR], 1.48; 95% confidence interval [CI], 0.96 to 2.28) and long-course therapy (OR, 1.45; 95% CI, 0.94 to 2.22) for recurrence and relapse of VAP. The findings were similar for VAP caused by NF-GNB (OR, 1.90; 95% CI, 0.93 to 3.33 vs OR, 1.76; 95% CI, 0.93 to 3.33). No difference was found between the two groups for 28 day-mortality, mechanical ventilation duration, number of extra-pulmonary infections, acquisition of MDR pathogens, and length of ICU stay. However, short-course therapy significantly increased the number of antibiotic-free days.
Tailored strategies (including clinical and biological endpoints) should be tested in RCTs.
The authors note that while the results suggest that short-course therapy for VAP is preferrable because it reduces exposure to antibiotics, the findings are limited by the small number of trials included in the meta-analysis, the heterogeneity of the studies, and the differences in antibiotics used by the two groups.
"Tailored strategies (including clinical and biological endpoints) should be tested in RCTs in order to individualize antibiotic duration treatment," they wrote.
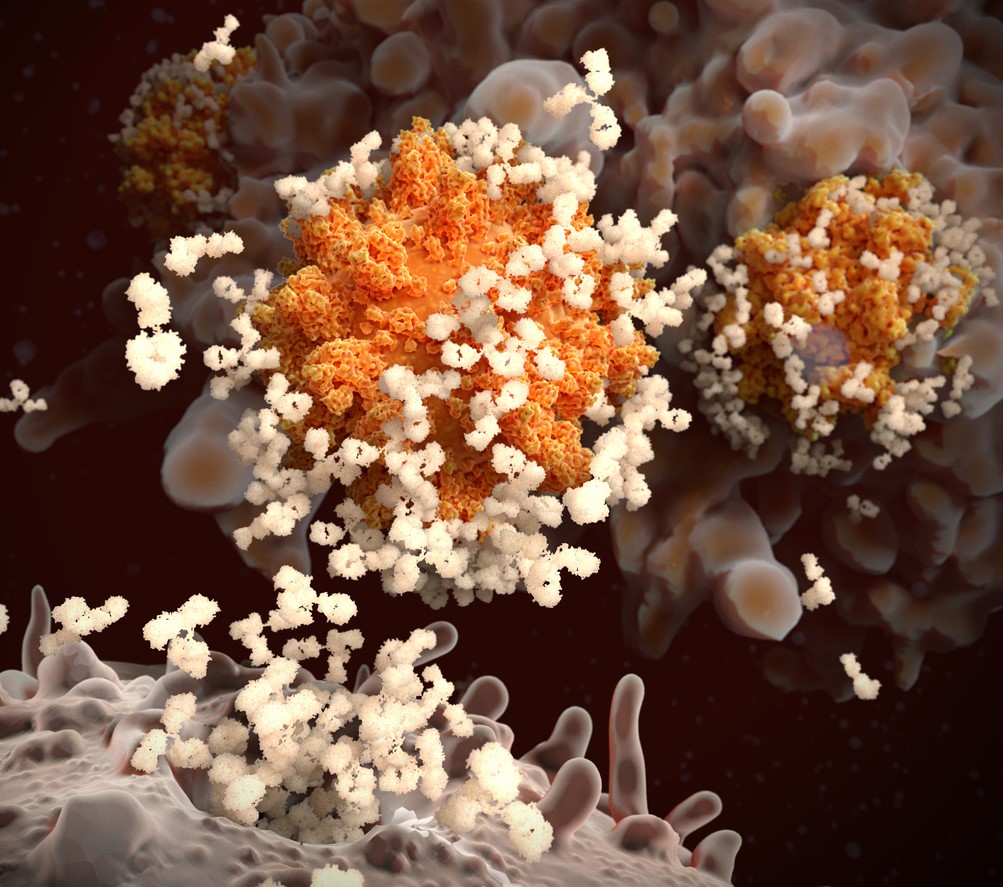 The monovalent (single-strain) COVID-19 vaccine booster was 74% effective against Omicron infection compared with the primary vaccine series for 3 months, but protection waned to 42% from 3 to 6 months and 36% after 6 months, estimates a
The monovalent (single-strain) COVID-19 vaccine booster was 74% effective against Omicron infection compared with the primary vaccine series for 3 months, but protection waned to 42% from 3 to 6 months and 36% after 6 months, estimates a 














