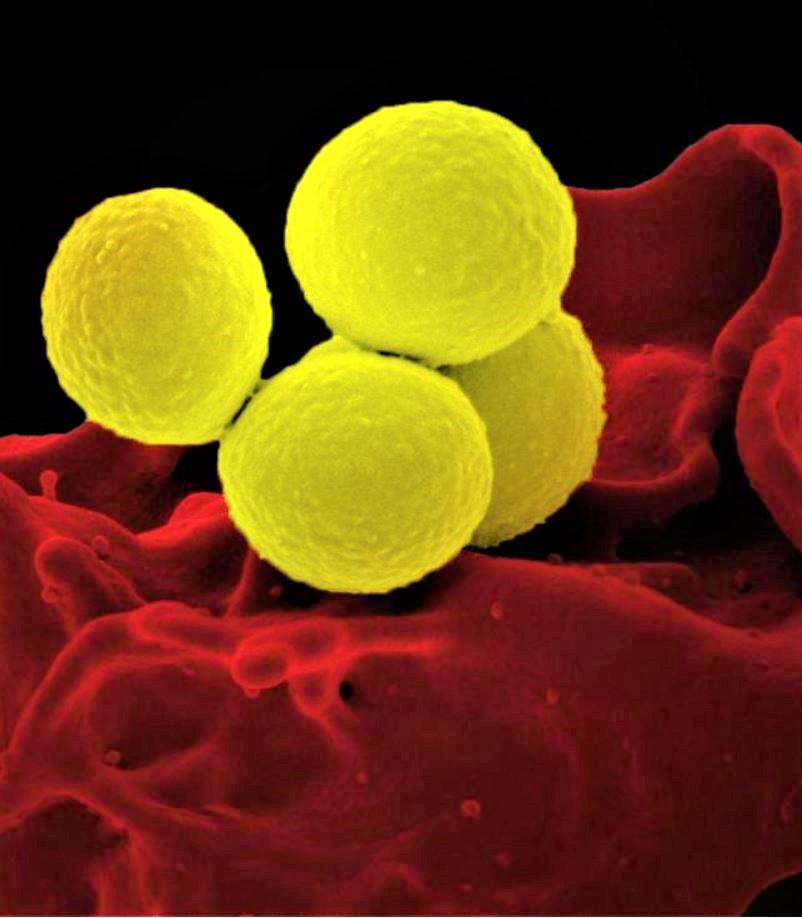
The addition of an antistaphylococcal beta-lactam to standard antibiotic therapy did not result in significant improvement for patients hospitalized with methicillin-resistant Staphylococcus aureus (MRSA) bacteremia, an international team of researchers reported today in JAMA.
The findings are from a randomized clinical trial conducted at 27 hospitals in four countries among patients hospitalized with MRSA bacteremia. The trial was stopped early because of safety concerns, as patients receiving combination therapy had significantly higher rates of acute kidney injury (AKI) than those who received standard therapy.
No significant improvement, higher kidney toxicity
The purpose of the trial, conducted by investigators with the Australasian Society for Infectious Diseases Clinical Research Network and dubbed CAMERA2 (Combination Antibiotics for Methicillin Resistant Staphylococcus aureus), was to test the hypothesis that combining an antistaphylococcal beta-lactam antibiotic with either daptomycin or vancomycin—the standard therapies for MRSA bacteremia—could improve outcomes in hospitalized adults. That hypothesis is based on in vitro research, animal studies, and small observational studies that have indicated a potential benefit.
The trial included 352 patients recruited from hospitals in Australia, Singapore, New Zealand, and Israel from August 2015 through July 2018. The patients were randomized 1:1 to receive the standard therapy or standard therapy plus an intravenous beta-lactam (flucloxacillin, cloxacillin, or cefalozin) for the first 7 days following randomization.
The primary outcome was a 90-day composite of mortality, persistent bacteremia at day 5, microbiologic relapse, and microbiologic treatment failure. Investigators aimed to detect a clinically meaningful absolute reduction of 12.5% in the primary end point. Secondary outcomes included all-cause mortality at 14, 42, and 90 days; persistent bacteremia at day 2 and 5; AKI; and microbiologic relapse and treatment failure.
Among the 345 patients (median age, 64) in the primary analysis, the investigators found no significant difference in the primary outcome between the two groups: The primary outcome occurred in 59 of 170 (34.7%) assigned to combination therapy and 68 of 175 (38.9%) who received standard therapy (absolute difference, -4.2%; 95% confidence interval, -14.3% to 6.0%; P = .42).
Analysis of secondary outcomes found that mortality did not significantly differ between the two treatment groups at any time, but persistent bacteremia at day 5 was less common in the combination therapy group (19 of 166, 11.4%) than in the standard therapy group (35 of 172, 20.3%), for an absolute difference of -8.9% (95% CI, -16.6% to -1.2%).
AKI, however, was significantly more common in the combination therapy group (34 of 145, 23.4%) than in those who received standard treatment (9 of 145, 6.2%) (absolute difference, 17.2%; 95% CI, 9.3% to 25.2%).
The difference in AKI between the two groups was first noticed by an independent data safety and monitoring board (DSMB) during an interim analysis of 220 patients in March 2018. After further analysis of data on 343 patients in July 2018 showed a significantly higher kidney toxicity in the combination treatment group, and no decrease in 90-day mortality, the DSMB recommended stopping recruitment.
The trial investigators say that even though the reduction in persistent bacteremia in patients who received combination therapy signaled potentially improved efficacy, the higher rates of AKI essentially erased that benefit.
"Given the early termination, the trial may have been underpowered to demonstrate an improvement in the composite primary end point; however, it is likely that any potential gains in efficacy with combination therapy would be offset by the increased toxicity," they write.
They add that the lack of benefit for combination therapy demonstrated in this trial and in previous clinical trials across a broad range of patients with S aureus bacteremia "should give pause to enthusiasm for combination therapy outside of clinical trials."
Limitations noted
Among the limitations noted by the investigators is that the results are largely limited to treatment with vancomycin plus flucloxacillin or cloxacillin, as daptomycin and cefazolin were infrequently used in the trial. In a post hoc analysis of the combination treatment group, 27% of patients (30 of 111) who received flucloxacillin or cloxacillin developed AKI, compared with 3.7% of patients (1 of 27) who received cefazolin.
Taking this into account, Tejal Gandhi, MD, and Preeti Malani, MD, of the University of Michigan, write in an accompanying editorial, the results raise the question of whether there are particular antibiotic combinations that could improve outcomes for MRSA bacteremia without increased toxicity.
"If so, could better outcomes be accomplished with more cost-effective regimens, such as vancomycin and cefazolin, compared with more expensive combinations, such as daptomycin and ceftaroline?" they ask.
Gandhi and Malani say that and other questions, including whether the source of bacteremia or the age or comorbidities of the patients influence the therapeutic strategy, deserve further investigation, since many MRSA bacteremia patients treated with standard therapy still experience treatment failure, and the associated mortality rate has remained at 20% to 25%. But for now, they conclude, combination therapy does not appear to be the answer.
"Until such data are available, routine combination therapy with a b-lactam as initial treatment for MRSA bacteremia should be avoided," they write.
See also:
Feb 11 JAMA abstract
Feb 11 JAMA editorial abstract