First in a two-part series examining the numbers and epidemiologic factors surrounding the virus many experts believe could lead to the next pandemic—and what they mean for your business.
(CIDRAP Source Weekly Briefing) – The apparent lull in avian flu cases may spell apathy for senior executives—even if it means nothing in terms of the danger posed by the H5N1 virus. Use this period to mobilize resources and educate management about why this is not the time to let down your guard.
A cursory look at the numbers tells one story.
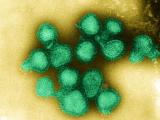
Fewer people are getting sick and dying from H5N1 avian influenza in 2007 than 2006. In the first 4 months of the year, 28 people have been reported and confirmed ill with the virus, down from 62 during the same period last year. News coverage of the deadly H5N1 virus has diminished, almost disappearing. And the pathogen's apparent lack of momentum coupled with its long-term presence have led many people to tune it out, file it away, or write it off as "public health's Y2K."
But a closer examination of the epidemiologic features of H5N1 tells a different, more ominous story.
The threat is not over—and won't be for the foreseeable future, according to scientists. The virus remains deadlier than the one responsible for the pandemic of 1918. H5N1's case-fatality rate (CFR), the ratio of how many people get sick from a disease to how many die of it, has remained steadily high—at about 60%—since it first emerged in 1997.
Weekly Briefing asked several influenza experts to put the current numbers of human H5N1 cases and deaths into context to help pandemic planners educate themselves and their senior executives about what these statistics really mean for the threat of a pandemic.
2007 statistics in context
So far this year, the World Health Organization (WHO) has confirmed 28 cases, 14 of them fatal, from the six countries that have reported them. But the numbers are too small to interpret in a meaningful way, says Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, Minneapolis, and Editor-in-Chief of Weekly Briefing. "The interpretation of 28 cases over such a short period of time doesn't mean anything at all," he says.
Just as a spike in cases cannot be interpreted as the start of the next pandemic, neither should a relatively quiet period be seen as the end of H5N1, he says.
Keiji Fukuda, MD, head of the WHO's Global Influenza Programme, agrees. "Progress in reducing poultry outbreaks is encouraging, but as long as H5N1 persists among poultry and other bird populations, it remains a danger to people and a highly concerning threat to initiate a pandemic," he says.
From Apr 1 to Apr 11, the last date the WHO updated its H5N1 cases, the organization confirmed only seven cases of H5N1. But April was a very quiet month in 2006 as well, with only five confirmed cases. Fukuda says variations in the number of cases are expected. "The H5N1 epidemiological patterns during the past few years have taught us to expect up and down patterns in H5N1 activity levels," he says. "It is clear that this virus has demonstrated its ability to persist for long periods of time and to reappear in places where strong control programs have been put in place. At this point, it is impossible to say the risk for a pandemic has decreased."
In addition, no one knows what the prelude to any pandemic looks like, because no one has ever tracked this type of prepandemic data, says Greg Dworkin, MD, editor of the Flu Wiki Web site, which tracks news and information about influenza. It's important not to make predictions about how the pandemic will unfold, its virulence, or the number of waves, he says. "Some people say 'if it's been around since 1997 in Hong Kong, isn't that a long time for the virus to not explode?' The answer is we don't know. As a wise pandemic expert once said 'if you've seen one pandemic, you've seen one pandemic.'"
In other words, no one knows whether H5N1 or another virus is going to cause the next pandemic, because viruses appear to follow no predictable pattern as they spread and jump species. For example, the avian influenza virus H3N8 jumped from birds to horses in 1963 and then to dogs—but not until 2004.
Looking at only the number of H5N1 poultry outbreaks and human cases in the short term to evaluate the pandemic threat is a mistake, says David Morens, MD, a scientist at the National Institutes for Health, Washington, DC. "It's spreading and will continue to spread," he says. "It's not going to go away. The virus is part of the environment, and it's likely to be where it is for the foreseeable future."
The recent relatively low number of cases, he says, could be due to saturation of the viral host, meaning that it has infected all the poultry it can possibly infect in a given area, and the poultry either died of the infection or were culled. On average, the life expectancy of a chicken is 35 to 40 days (from hatch to plate). When new, susceptible birds are added to the population, the resultant group has no immunity. Thus, when the virus is reintroduced, it is able to infect a large number.
Or, Morens says, the low number of cases could be due to educational efforts to inform people how to stop the disease. "You're seeing that learning curve," he says. "So many new communities have had these experiences that there's perhaps a combination of saturation and a high level of information that allows people to stop transmission."
The number of human deaths attributed to H5N1 (172 worldwide), although no doubt a tragedy for the victims' families, is small from a public health standpoint, Morens says. At the same time, no one knows how H5N1 might jump from poultry to humans—or whether another, different virus will emerge to cause the next pandemic. "What we worry about is that this virus might in the future become a pandemic virus," he says. "We don't know if the turning of this virus into a pandemic virus is possible, and, if it is, we don't know what it would take to make it happen."
Stable case-fatality rate
The CFR remains high, at 60%. It has hovered between 50% and 75% since February 2004. "It's a very high case-fatality rate," Dworkin says. "For those hoping that the case-fatality rate would drop over time, that's not been seen."
For comparison, the CFR of the 1918 influenza pandemic was 2.5%. "While not predicting an H5N1 pandemic, I think that it [the CFR] is an important statistic to keep in mind for planners who are charged with thinking about worst-case scenarios," he says.
H5N1 in Indonesia
To further confound things, the official numbers of human infections and deaths from the WHO are misleading, because Indonesia has not been sharing samples of what it has identified as H5N1 since Jan 29, 2007. About one third of the world's H5N1 cases have occurred in Indonesia. Of Indonesia's cases, the WHO has confirmed only six this year, five of them fatal. If the unconfirmed Indonesian cases were included, they would boost Indonesia's 2007 cases to 20 and its deaths to 17—more deadly than that country's 2005 statistics (20 cases, 13 deaths).
Indonesian health officials are not cooperating with the WHO, having called into question the fairness of the WHO and pharmaceutical companies' using Indonesian virus samples to produce vaccines the country may not be able to obtain or afford. As a result, the WHO has not recognized Indonesia's H5N1 cases since Jan 29, because the organization cannot confirm the results in an independent lab.
If Indonesia resumes sharing H5N1 samples, Fukuda says that WHO labs will test any H5N1 samples provided by Indonesia, which will allow the labs to confirm the infections and include all such H5N1 cases in the WHO statistics. "Alternatively, a lab in Indonesia may demonstrate that it meets the WHO guidelines for H5N1 testing so that the results from Indonesia can be accepted without the need for further verification," he says. "Even if a country's laboratory is able to verify H5N1 virus infection, this does not remove the importance of Indonesia and all other countries sharing their H5N1 viruses for risk assessment for vaccine strain selection and development purposes."
Other confounding factors
Several factors cloud the accuracy and reporting of data, including problematic data collection, the impact of using antivirals, and a lack of data from previous pandemics.
Problematic data collection. In general, countries affected by H5N1 have moved toward more complete reporting, but Indonesia is notable because it has purposefully withheld its H5N1 viruses and sought publicity over this action to highlight the need to improve access to H5N1 and pandemic vaccines for all countries, Fukuda says. "WHO is in complete agreement with the need for more equitable access to these resources but also believes that all countries should, at the same time, support global surveillance, including virus sharing, for influenza," he says. "For influenza, even Indonesia acknowledges the importance of virus sharing for the purpose of mutual protection against this threat."
Antiviral use. Treating a patient with the antiviral oseltamivir (Tamiflu) can suppress viral growth, potentially resulting in a false-negative test for H5N1, Dworkin says. If, for example, a patient with suspected H5N1 is hospitalized, given Tamiflu, and then tested for H5N1 and the result is negative, the patient's case would not be recorded as positive—even though the patient may truly be infected with H5N1.
Lack of historical data. Predicting the course of a pandemic also is difficult, given incomplete or nonexistent data collection from previous pandemics, according to Dworkin. "What we really need is a complete and total understanding of the natural history of pandemics, from the time that they start to the time that they're over," he says. "We simply need to be prudent about what we do know," which at this time is that H5N1 is still making people ill and recurring in the bird population, its spread may be related to the commercial poultry industry and the smuggling of poultry, and it has a high CFR.
H5N1 in birds
Joseph Domenech, chief veterinary officer of the Food and Agriculture Organization (FAO) of the United Nations in Rome, reports fewer H5N1 outbreaks in poultry—the main source of the virus—this year than at the same time last year. He also says that although many countries have managed to contain the virus through quick action, the threat of H5N1 gaining efficiency in human-to-human transmission has not disappeared. "Globally, the situation is a lot better," he says of H5N1 infection in poultry. "A lot of countries have been able to get rid of the disease, but it doesn't mean that we are satisfactory and there is no reason to worry. There are still a lot of reasons to worry."
In 2007, H5N1 has affected poultry in 17 countries. Four countries reported their first-ever poultry outbreaks this year: the United Kingdom (Jan 27), Bangladesh (Feb 5), Saudi Arabia (Mar 12), and Ghana (May 2). Others, such as Cambodia, Laos, and Turkey, have seen reintroduction of the virus. The FAO is paying especially close attention to Bangladesh for spread of the virus, Domenech says.
Turkey, Thailand, and Vietnam, which had been areas of concern, have done a good job curbing the virus, he says. However, he adds that Indonesia, Egypt, and, to a lesser extent, Nigeria remain H5N1 hot spots.
Indonesia, he says, is of particular concern because:
- Only three of Indonesia's 33 provinces remain free of H5N1 infection in poultry.
- The country has the world's highest human death toll from H5N1 (63 WHO-confirmed deaths, plus 12 more unconfirmed deaths).
"The risk of a human pandemic is still the same," he says.
Take the long view
While the number of human H5N1 cases may be slightly lower this year than at the same time last year, experts say that meaningful interpretation of such a small number of cases over a few months isn't possible.
Companies most likely to come through a pandemic intact, say experts, are ones that take the long view. Whether it's caused by H5N1 or a different virus, another pandemic will occur—and businesses need to be ready for it. As Fukuda says: "What is clear is that actions to prepare for a pandemic need to continue."