Polish researchers publishing today in Scientific Reports suggest that patients receiving antiplatelet therapy before contracting COVID-19 were less frequently hospitalized in the intensive care unit (ICU), developed shock less often, and had lower 3-month mortality. The study was conducted in 2020 and 2021, before the widespread use of vaccine in Poland.
The study compared outcomes among hospitalized COVID patients who were taking antiplatelet therapy prior to infection (274 patients) and matched controls who had never received antiplatelet therapy.
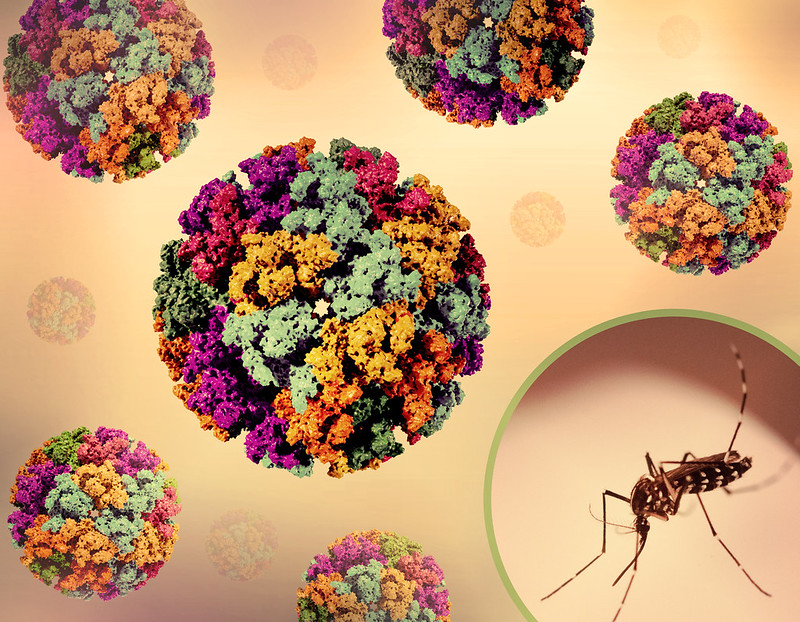
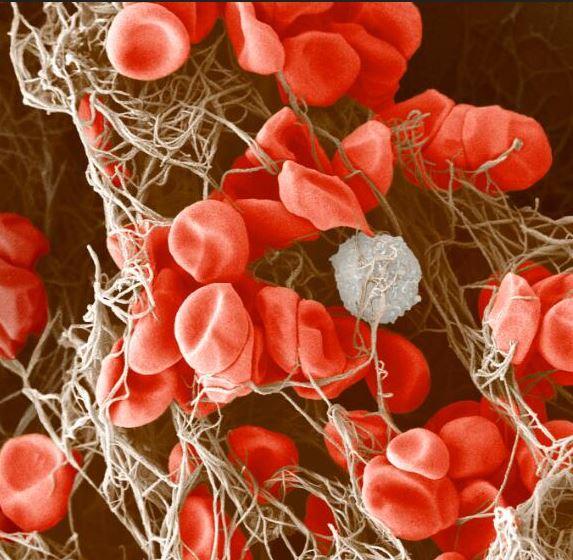
Thrombosis, or blood clotting, has been indicated as a factor in COVID-19 mortality, and the authors hypothesized that antiplatelet therapy may protect against severe outcomes linked to thrombosis, as platelets play a major role in hemostasis, thrombosis, and inflammatory response, they said.
In the study, 94% of patients were taking a form of acetylsalicylic acid, including aspirin, at the time of COVID infection.
3-month mortality better in antiplatelet group
In-hospital mortality for both groups of patients was similar, with deaths occurring among 53 (19%) and 64 (23%) of the antiplatelet therapy and no-antiplatelet groups, respectively.
Patients who had been on antiplatelet therapy, however, were less likely to go to the ICU (9% vs 15%), and develop shock (9% vs 15%). There was also a lower 3-month mortality (31% vs 39%) for the antiplatelet therapy group (hazard ratio 0.69, 95% confidence interval, 0.51 to 0.93.)
More cardiovascular events were reported in the short- and long-term in the antiplatelet therapy group, but the authors suggest this is likely due to preexisting comorbidities.
The overall prognosis was better in the AP [antiplatelet] group.
"Despite the greater number of comorbidities and vascular events during hospitalization, the overall prognosis was better in the AP [antiplatelet] group," the authors wrote.
.