New data from the World Health Organization (WHO) indicate that resistance to the only remaining treatment for gonorrhea is emerging globally, and that widespread treatment failure is likely in the coming years unless new antibiotics are developed.
"It will only be a matter of time," Teodora Wi, MD, a medical officer with the WHO's Department of Reproductive Health and Research, told reporters.
Wi is the lead author of a study today in PLoS Medicine that details the extent of the problem. In the study, data from 77 countries reporting to the WHO Global Gonococcal Antimicrobial Surveillance Programme (WHO GASP) show increasing resistance to azithromycin and emerging resistance to the extended-spectrum cephalosporins (ESCs) cefixime and ceftriaxone—the drugs that make up the last-line treatment for gonorrhea.
To date, three countries—Japan, France, and Spain—have reported "superbug" strains of gonorrhea that are resistant to all current forms of treatment.
An accompanying commentary in PLoS Medicine by many of the same authors laid out a plan to accelerate the development of new antibiotics for treatment of gonorrhea and evaluate possible treatments using existing drugs.
A 'very smart bug'
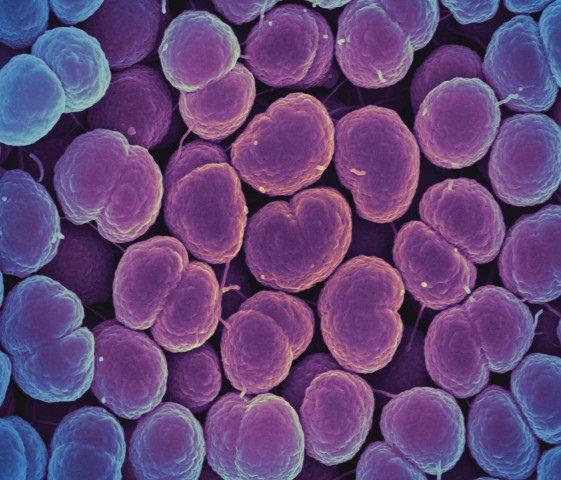
The WHO estimates there are currently 78 million global cases of gonorrhea, which is caused by the Neisseria gonorrhoeae bacterium. Gonorrhea spreads through unprotected vaginal, oral, and anal sex and can infect both men and women. It generally causes infections in the genitals, rectum, and throat, and pregnant women can pass the infection to their newborns during childbirth. Serious and permanent health problems, including pelvic inflammatory disease and infertility, can result if the disease goes untreated.
"There are many consequences of not treating gonorrhea," Wi said.
But treating gonorrhea appropriately has become a challenge, because the bacterium's DNA has shown the ability to quickly mutate and develop resistance to every antibiotic that's been used to treat it. "Gonorrhea is a very smart bug," Wi said. "Every time you introduce a new class of antibiotics to treat gonorrhea, the bug becomes resistant to these antibiotics."
As the data from WHO GASP indicate, that's what appears to be happening with cefixime and ceftriaxone, the drugs that the WHO currently recommends be used in combination with azithromycin for treatment of most gonococcal infections.
According to the data, which cover 2009 through 2014, isolates from 55 of the 77 countries reporting (66%) showed resistance or decreased susceptibility to cefixime or ceftriaxone. In 26 of those countries, the percentage of resistant isolates was at least 5% or higher—the level at which the WHO recommends discontinuing use of an antimicrobial in empiric treatment. In addition, the GASP data showed that 81% of countries reported resistance or decreased susceptibility to azithromycin.
Wi called the GASP data the "tip of the iceberg" and noted the extent of the problem could be much greater, since most of the data are from high-income countries with good surveillance systems. In low-income countries in Africa, Central Asia, and the eastern Mediterranean region, where sexually transmitted infection (STI) rates tend to be higher, appropriate laboratory tests and data on drug-resistant gonorrhea are insufficient. Wi said it is likely that cases of untreatable gonorrhea exist in these countries, "and they are not likely being documented at this point."
Emergence of untreatable gonorrhea
This rising resistance to the currently recommended treatment, Wi said, means "we are soon going to be seeing the threat of untreatable gonorrhea in the future," since drug-resistant gonorrhea can quickly become widespread once it starts getting transmitted. Wi could not say how many years it would take for widespread untreatable gonorrhea to emerge.
In June 2016, the New England Journal of Medicine reported on the failure of ceftriaxone and azithromycin therapy in a man from the United Kingdom diagnosed as having gonorrhea. This was the first reported failure of dual therapy in Europe. The N gonorrhea strain identified in the man was identical to a strain spreading in Japan that has shown reduced susceptibility to ceftriaxone and azithromycin.
In September 2016, public health officials in Hawaii reported a cluster of N gonorrhea isolates from seven people that showed high resistance to azithromycin and reduced susceptibility to ceftriaxone—the first such cases reported in the United States. All seven patients were successfully treated.
The GASP data also showed that 97% of countries reported resistance to ciprofloxacin, a fluoroquinolone that is no longer recommended for gonorrhea treatment but is still being used in some African countries.
Wi added that, in addition to gonorrhea's innate ability to mutate, increasing resistance is also a result of inappropriate antibiotic treatment, which occurs when the wrong dosage of drugs is prescribed, treatment directions aren't properly followed by patients, or poor-quality drugs are used.
Lack of treatment alternatives
A lack of alternatives to the currently recommended treatment for gonorrhea makes the issue more pressing. The three antibiotic candidates currently in the pipeline—solithromycin, zoliflodacin, and gepotidacin—are in various stages of clinical development, but none are guaranteed to make it to market, Manica Balasegaram, MRCP, MSc, director of the Global Antibiotic Research and Development Partnership (GARDP), told reporters.
"The situation is, actually, fairly grim," he said.
Balasegaram, lead author of a paper that lays out a roadmap for research and development of drug-resistant gonorrhea treatments, said GARDP's strategy includes four components: Accelerating the development of drugs in the pipeline, evaluating the ability of existing antibiotics to treat gonorrhea (either alone or in combination with other drugs), exploring ways to improve the administration of gonorrhea treatment, and supporting the development of simplified treatment guidelines.
As part of this strategy, Balasegaram announced that GARDP had entered into a partnership with biotech company Entasis Therapeutics to accelerate development of zoliflodacin by helping register and conduct public health trials. Balasegaram also said GARDP would also play a role in guiding stewardship efforts for any new gonorrhea treatments. "A critical part of our work will not just be to do the research and development, but also to guide appropriate long-term use, while ensuring access," he said.
Wi said that in addition to finding new treatments for gonorrhea, scientists must focus more on developing affordable, point-of-care tests that can quickly and correctly diagnose gonorrhea. While many people who become infected don't show any clinical symptoms and as a result go untreated, others may show symptoms (such as vaginal or urethral discharge) but have a different type of infection. Since antibiotic treatment in low-income settings is often based on these visible symptoms, inappropriate antibiotic treatment can result.
Prevention is another strategy the WHO is pursuing. That includes development of a preventive vaccine, which Wi said has been hampered by the inability to find the right antigen for preventive immunity, and promotion of safer sex behaviors, including increased condom use. The WHO has set a goal of a 90% reduction in gonorrhea incidence by 2030.
See also:
July 7 PLoS Medicine study
July 7 PLoS Medicine commentary