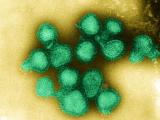
Apr 13, 2010 (CIDRAP News) – About one in every eight residents of Singapore became infected with novel H1N1 influenza during the 2009 pandemic's main wave there, according to blood sampling done as the outbreak proceeded, with higher infection rates among members of the military and much lower ones among healthcare workers.
Writing in tomorrow's Journal of the American Medical Association (JAMA), public health and academic experts from Singapore and Australia say the low average rate of 13% seroconversion means that "most of the adult population likely remained susceptible" after the pandemic wave passed, and therefore would be vulnerable to the flu's return.
Meanwhile, a letter in Emerging Infectious Diseases (EID) by Singaporean and Australian researchers, who include two authors from the JAMA paper, says that among 50 older adults checked for flu immunity before the pandemic's arrival, none had cross-reactive antibodies that would have protected them from infection by the pandemic strain.
That finding confirms those by other teams that older adults in Asia seem to lack the cross-reactive immunity apparently possessed by those in the West who were exposed before 1958 to the last naturally circulating H1N1 strain descended from the pandemic virus of 1918. But it raises intriguing questions about the results published in JAMA, which found lower levels of seroconversion from infection among those older than 40—though that finding was not uniform across all the cohorts in the study.
The JAMA study was launched before the pandemic's August 2009 first wave in Singapore, and relied on blood samples taken in late June, late August–early September, and late September–early October. It used four separate large cohorts: 1,213 members of the military, 558 staff from a large hospital, 300 residents of long-term care facilities, and 838 members of a "cohort of cohorts" drawn from a long-term research study on community health, some of whose baseline samples dated back to 2005.
As a correlate of infection and subsequent immunity, the team used the widely accepted benchmark of a fourfold or greater increase in antibody titers using a hemagglutination inhibition assay.
Overall, 13% of the community cohort, 29% of the military cohort, and 7% of the hospital staff cohort seroconverted in an analysis detailed in the journal. (The long-term care residents were assessed separately because their baseline samples were drawn later than the other groups.)
Among the community members, the highest rates of seroconversion were among those aged 20 to 24 (21%) and the lowest among those older than 60 (8%). Among the military, who were overwhelmingly younger than 24, 44% of those 15 to 19 seroconverted, compared with 1 member each of the small groupings of those 50 to 59 and older than 60.
Hospital workers, though, had lower seroconversion rates in all age-groups, from 6% among those 20 to 24 to 4% among those 30 to 39 to a single member of a small group of those older than 60.
The authors hypothesize that healthcare personnel may have been protected from infection by practices instituted at the local start of the epidemic, including patient and visitor screening and wide use of personal protective equipment.
The high rates of infection among young military members, they add, demonstrate the increased vulnerability of the young to the novel H1N1 strain, and also underline that "special preventive measures" should be considered in the future for similar groups whose age and living conditions may subject them to greater intensity of transmission.
Despite the findings in the JAMA study of low rates of infection among the elderly, the EID study shows a paradoxical lack of pre-existing cross-reactive immunity in the small cohort of 40- to 80-year-old adults sampled before the pandemic's arrival. It raises the possibility, referenced in the JAMA paper, that reduced susceptibility as a result of age may have played a role in low infection rates among all the groups of elderly assessed.
The EID authors say that differences in urban and rural study populations, and in previous use of seasonal flu vaccine in different countries, may also have played a role.
Chen MIC, Lee VJM, Yen W-Y, et al. 2009 Influenza A(H1N1) seroconversion rates and risk factors among distinct adult cohorts in Singapore. JAMA 2010 Apr 14;303(14):1383-91 [Abstract]
See also:
Tang JW, Tambyah PA, Wilder-Smith A et al. Cross-reactive antibodies to pandemic (H1N1) 2009 virus, Singapore. (Letter) Emerg Infect Dis. 2010 May (early online publication) [Full text]