Jul 13, 2011 (CIDRAP News) – A five-country study from Europe indicates that the use of adjuvanted vaccines against the pandemic H1N1 influenza virus probably did not increase the risk of Guillain-Barre syndrome (GBS), but the investigators could not firmly rule out a slightly greater chance of suffering the paralytic condition.
Writing in BMJ, the European researchers report that the adjusted odds ratio (OR) for GBS in those who were vaccinated was 1.0, indicating no higher risk, but the 95% confidence interval (CI) was 0.3 to 2.7, leaving the possibility open.
"The risk of occurrence of Guillain-Barre syndrome is not increased after pandemic influenza vaccine, although the upper limit does not exclude a potential increase up to 2.7-fold or three excess cases per one million vaccinated people," the report states.
GBS associated with flu vaccination has been a concern since the aborted US swine flu vaccination campaign of 1976, when almost one extra GBS case was reported per 100,000 vaccinations. Since then, studies of seasonal flu campaigns have shown no increase or only a slightly increased risk of 1 to 2 extra cases per million vaccinees, according to an editorial accompanying the BMJ report.
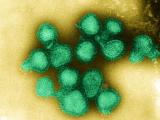
In Europe, the 2009 pandemic triggered the first widespread use of flu vaccines containing adjuvants: GlaxoSmithKline's Pandemrix and Novartis's Focetria, which were the most widely used vaccines there. The public's unfamiliarity with adjuvants has been cited as a factor in the generally low vaccine uptake during the pandemic in Europe. Adjuvants have not been used in US flu vaccines.
The European study was a case-control investigation conducted in Denmark, France, the Netherlands, Sweden, and the United Kingdom by the Vaccine Adverse Events Surveillance & Communication (VAESCO) consortium. The study period was November 2009 through March 2010.
The researchers identified GBS cases, matched each patient with up to 25 controls by age, sex, onset date, and country, and sought to determine whether they had received an H1N1 vaccine within 6 weeks before the date of GBS onset.
They identified 154 GBS cases and managed to match 104 of them with one or more controls. Most of the case-patients were men between the ages of 46 and 61. Six of the patients required mechanical ventilation or died of the condition.
Pandemrix was the most widely used pandemic vaccine in the study population, the report says. Vaccine uptake was highest in the Netherlands and Sweden and much lower—less than 10%—in the UK, Denmark, and France.
The investigators found that the unadjusted ORs for GBS ranged from 1.3 to 2.5 in the UK, Sweden, and the Netherlands. In Denmark the adjusted OR was 9.5 on the basis of just two cases, while the risk for France could not be estimated because there was only one vaccinated case-patient and no vaccinated controls.
However, the apparent increase in risk largely disappeared when the researchers adjusted for flu-like illness or upper respiratory tract infection and seasonal flu vaccination in their subjects. Those adjustments yielded the OR of 1.0 (95% CI, 0.3 to 2.7).
The authors say that with the "apparent strong confounding" effects of flu-like illness and seasonal flu vaccination, they could find no increase in GBS risk in a source population of around 50 million people in Europe.
They add, "Based on the 95% confidence interval for the adjusted odds ratio it is unlikely that the relative risk is above 2.7. Thus it is unlikely that there would be more than one excess case" of GBS per 340,000 people, or 3 per million. They note that this is well below the risk increase seen with the 1976 US swine flu vaccine.
The researchers say they are working on a larger study that will include cases from additional countries and cover a longer period.
In the accompanying editorial, four specialists with the US Centers for Disease Control and Prevention (CDC) describe the findings as being in accord with studies on the GBS risk associated with nonadjuvanted pandemic H1N1 vaccines but as puzzling in some respects.
"Overall, the results suggest that if there was an increased risk associated with the adjuvanted 2009 H1N1 vaccines studied, it was considerably smaller than that seen with the 1976 flu vaccines," they write. "Whether there was an increased risk, however, is not clear."
The CDC writers note that a large study of unadjuvanted H1N1 vaccinations in the United States indicated that the GBS risk was increased by less than one excess case per million vaccinations, but the researchers did not adjust for respiratory illnesses.
The commentators, led by Frank DeStefano, say respiratory illnesses have not previously been identified as a strong confounder for the association between seasonal flu vaccines and GBS. They suggest the confounding was more apparent in this study because vaccination occurred while the pandemic virus was circulating.
Dieleman J, Romio S, Johansen K, et al. Guillain-Barre syndrome and adjuvanted pandemic influenza A (H1N1) 2009 vaccine: multinational case-control study in Europe. BMJ 2011 Jul 12;343 [Full text]
DeStefano F, Vellozzi C, Schonberger LB, et al. Safety of adjuvanted pandemic influenza A (H1N1) 2009 vaccines. (Editorial) BMJ 2011 Jul 12;343 [Extract]
See also:
Jan 15, 2010, CIDRAP News story on adjuvanted vaccines in Europe
Jun 2, 2010, CIDRAP News story on CDC report on GBS risk with H1N1 vaccine