 Two years into the COVID-19 pandemic, US cancer screening rates still hadn't recovered to pre-crisis levels, putting millions at risk for missed diagnoses, according to a study published yesterday in the Journal of Clinical Oncology.
Two years into the COVID-19 pandemic, US cancer screening rates still hadn't recovered to pre-crisis levels, putting millions at risk for missed diagnoses, according to a study published yesterday in the Journal of Clinical Oncology.
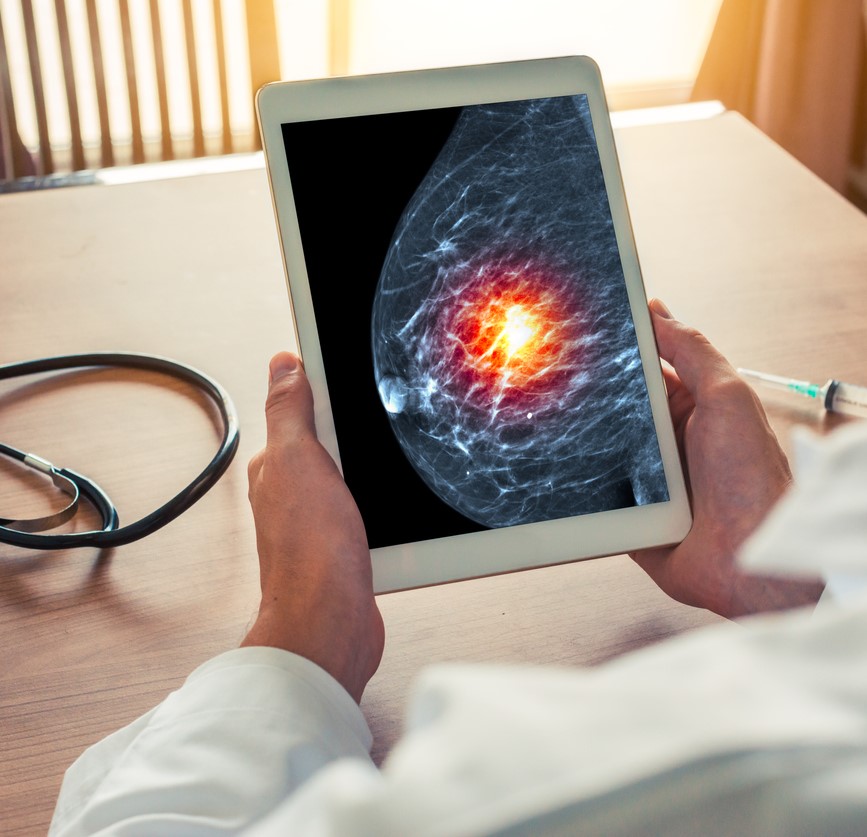
American Cancer Society (ACS) researchers used data from the 2019 and 2021 National Health Interview Survey to estimate the number of US Preventive Services Task Force (USPSTF)-recommended breast, cervical, prostate, and colorectal cancer screenings performed after the pandemic began.
The USPSTF recommends screening for breast cancer for women aged 50 to 74 years, cervical cancer for women aged 21 to 65 who have not had a hysterectomy, prostate cancer for men aged 55 to 69, and colorectal cancer for men and women aged 50 to 75.
Fewer breast, cervical, prostate screenings
From 2019 to 2021, past-year screenings declined from 59.9% to 57.1% for breast cancer, from 45.3% to 39.0% for cervical cancer, and from 39.5% to 36.3% for prostate cancer. Asian adults saw the biggest declines, ranging from -25% for breast cancer to -50% for prostate cancer.
The percentages translate to missed screenings for roughly 1.1 million women for breast cancer, 4.4 million women for cervical cancer, and 700,000 men for prostate cancer.
Colorectal cancer screening didn't change, because past-year at-home stool testing increased from 7.0% to 10.3%, offsetting the drop in colonoscopy from 15.5% to 13.8%. Although about 1.3 million fewer adults received a colonoscopy, 3.6 million completed stool testing, for a net gain of 1.5 million. Increases in stool testing were most pronounced among Black (66%) and Hispanic (82%) adults and those with low socioeconomic status (52%).
It's critical to get people back into their doctor’s offices to help prevent and catch cancer at its earliest stages.
The authors said that the increases in at-home stool testing among Black and Hispanic patients may have helped reduce racial and socioeconomic disparities in colorectal cancer screening, although positive tests still require follow-up colonoscopy.
"It's critical to get people back into their doctor’s offices to help prevent and catch cancer at its earliest stages when it might be easiest to treat," lead author Jessica Star, MA, MPH, said in an ACS news release.
 Surges in COVID-19 cases in the United States were associated with increased outpatient antibiotic prescribing in adults in 2020, according to an
Surges in COVID-19 cases in the United States were associated with increased outpatient antibiotic prescribing in adults in 2020, according to an 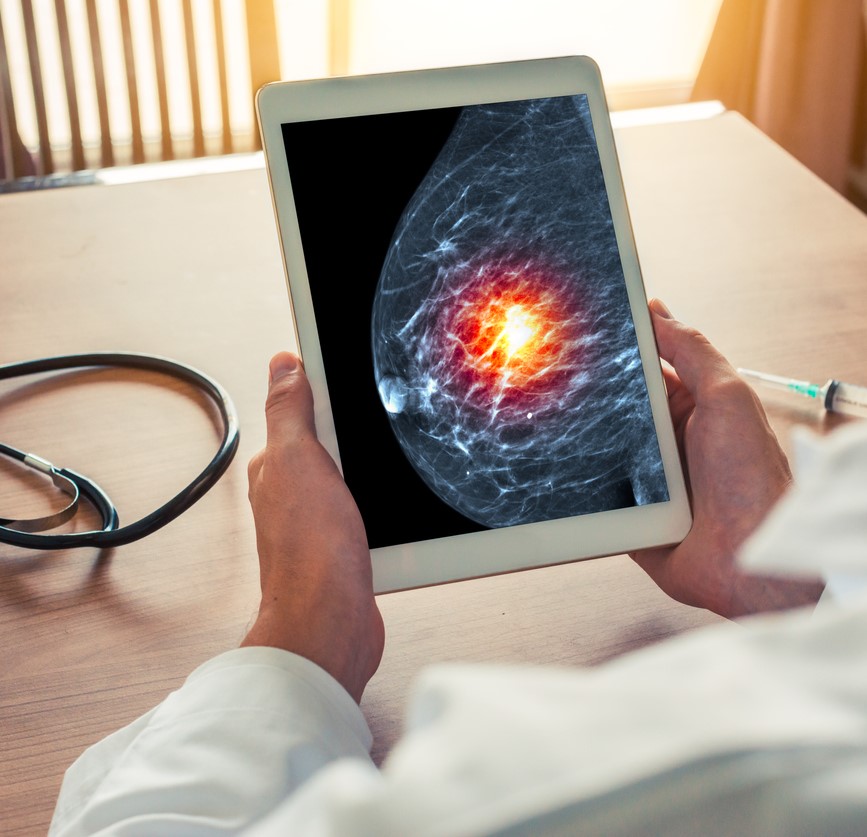 Two years into the COVID-19 pandemic, US cancer screening rates still hadn't recovered to pre-crisis levels, putting millions at risk for missed diagnoses, according to a
Two years into the COVID-19 pandemic, US cancer screening rates still hadn't recovered to pre-crisis levels, putting millions at risk for missed diagnoses, according to a 










