Apr 11, 2011 (CIDRAP News) A team of US researchers recently added to the evidence that humans can and do produce antibodies that target a wide range of influenza strains, though how the findings can be exploited in the quest for a "universal" flu vaccine remains to be seen.
The researchers tested serum samples from participants in an H5N1 flu vaccine study and also looked in a commercial preparation of intravenous immunoglobulin (an antibody preparation made from blood plasma and used to treat certain diseases). In both cases they found low levels of broadly neutralizing influenza A antibodies, including antibodies covering both of the major influenza A groups.
"These datato our knowledge, for the first timequantitatively show the presence, albeit at low levels, of two populations of heterosubtypic BnAbs [broadly neutralizing antibodies] against influenza A in human serum," says the report in the Apr 15 issue of Clinical Infectious Diseases (CID). The research team included members from several institutions in Boston; La Jolla, Calif.; and the National Institute of Allergy and Infectious Diseases in Maryland.
In an accompanying CID editorial, two leading flu experts from the Centers for Disease Control and Prevention (CDC) called the findings "auspicious" for the development of a universal flu vaccine.
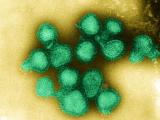
Flu vaccines now in use target the head of the flu virus's hemagglutinin (HA) protein, which evolves rapidly to evade the immune system, producing an ever-shifting spectrum of viral strains. Consequently the vaccine is reformulated each year in an effort to match the circulating viruses.
The prime goal of flu vaccine researchers is to develop a vaccine that targets a more stable region of the virus, so that one dose could provide protection against many strains and last many years.
Previous studies have yielded some evidence that humans produce broadly targeted flu antibodies in certain circumstances, but the new study suggests, according to the CDC experts, that such antibodies are part of the normal immune response to flu.
The investigators aimed to identify antibodies to a wide range of influenza A viruses, including both phylogenetic groups. Influenza A viruses come with 16 different subtypes of HA. Group 1 includes H1, H2, H5, H6, H8, H9, H11, H12, H13, and H16, while group 2 includes H3, H4, H7, H10, H14, and H15. Common seasonal flu viruses include 2009 H1N1, from group 1, and H3N2, from group 2 (in addition to influenza B).
The investigators analyzed pre- and post-vaccination serum samples from 77 participants in a trial of an H5N1 flu vaccine, looking specifically for antibodies to H1, H3, H5, and H7 viruses, and they also searched for antibodies similar to a known broadly neutralizing monoclonal antibody, called F10, which targets a stable region on the stem of the HA protein rather than its head.
Both the pre- and post-vaccination samples were found to contain antibodies to H3, H5, and H7 HAs, the report says. The post-vaccination samples showed an increase in H5 and H7 antibodies but not in H3 antibodies. In addition, the team found evidence of F10-like antibodies in both sets of samples, with the titer increasing 1.5-fold after vaccination in a majority of the volunteers.
In the other part of the study, the investigators looked for antibodies in commercially prepared intravenous immunoglobulin (IVIG) derived from thousands of plasma donors. The team's technique involved the use of magnetic beads to immobilize HA from a 2004 H5N1 virus collected in Vietnam to purify F10-like and anti-H5 antibodies from the IVIG. Few or none of the plasma donors would've been expected to have any immunity to H5 viruses, since H5N1 vaccines have been used only in clinical trials, and H5N1 infections have not been reported in the United States.
The researchers found evidence that about 0.01% of the IVIG consisted of H5 antibodies and that about 0.001% consisted of F10-like antibodies. Further, they found that these H5 antibodies reacted with H1, H3, and, to a lesser extent, H7 viruses. The F10-like antibodies bound to H1 and H5 (group 1) viruses, but not to H3 and H7 (group 2).
"We show that prevaccination serum samples have baseline heterosubtypic HA Ab [antibody] binding activity to both group 1 and 2 HA subtypes including H5 and H7, to which these subjects are most likely unexposed because of their US geographic location," the report says.
The authors say their findings don't answer whether the levels of either group 1 or group 2 antibodies they found would actually prevent illness, but the quantitative data suggest that the levels are borderline or below "titers that would traditionally be considered protective."
They also say the origins of the cross-reactive antibodies are a mystery. But the H5N1 vaccine study participants and the IVIG donors probably had been exposed to Group 1 (H1N1) and Group 2 (H3N2) viruses through vaccination or infection, and this may have given rise to H5- and H7-binding antibodies, the authors speculate.
In the CID editorial, Ruben O. Donis and Nancy J. Cox of the CDC say the finding that H5N1 vaccine induced F10-like antibodieswhich competed with F10 in biding to its target on the H5 HA stemsuggests that the volunteers developed broadly neutralizing antibodies to group 1 viruses as a result of H5N 1vaccination. They also hailed the researchers "remarkable" technique for finding F1-like antibodies in the IVIG.
""The observation that neutralizing antibodies to epitopes presenting in multiple HA subtypes . . . are part of the normal human immune repertoire is auspicious for universal influenza vaccine development, because it implies that broad protection may be elicited by enhancing the immunodominance of epitopes [sites] on the stem of engineered HA antigens," Donis and Cox write. They add that this approach is currently being "intensively investigated" in academic, government, and industry labs.
The study also drew praise from virologist Vincent Racaniello, PhD, Higgins professor in the Department of Microbiology & immunology at Colombia University. Racaniello, author of Virology Blog, commented that the existence of human monoclonal antibodies that target the HA stem and neutralize a broad range of flu viruses was already known.
He described the researchers' method of purifying antibodies from the IVIG as very clever. "These antibodies can neutralize both H5 and H1 viral strains in vitro," he told CIDRAP News by e-mail. "This observation is exciting because it shows that people can make broadly neutralizing antibodies. However, the authors have not shown that such antibodies can protect against infection in animals. More importantly, the antibodies are very rare0.001% of total immunoglobulin. Why people don't make more of these antibodies isn't clear, and understanding that will be important if we are going to try to induce such antibodies by immunization."
Racaniello added that several previous studies have shown that broadly neutralizing antibodies can be generated in animals by immunizing them with an HA-stem vaccine or by prime-boost vaccination. Those findings raised the "exciting" prospect of a broadly protective flu vaccine within the next decade.
"The current study shows that people can make such antibodies, which is also important," he said. "How such findings will be translated into a vaccine isn't known, but trial and error with different antigens and methods of presentation, including the use of adjuvants, will likely be productive."
Sui J, Sheehan J, Hwang WC, et al. Wide prevalence of heterosubtypic broadly neutralizing human anti-influenza A antibodies. Clin Infect Dis 2011 Apr 15;52(8):1003-9 [Abstract]
Donis RO, Cox NJ. Prospecting the influenza hemagglutinin to develop universal vaccines. (Editorial) Clin Infect Dis 2011 Apr 15;52(8):1010-12 [Extract]
See also:
Jan 14 CIDRAP News story "Antibodies from H1N1 patients raise hope for more versatile flu vaccines"