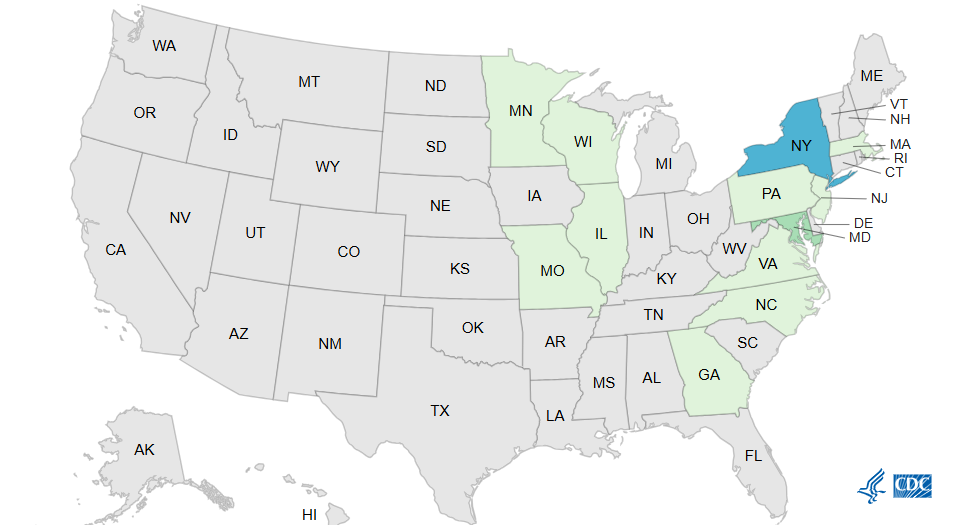
The US Centers for Disease Control and Prevention (CDC) report a 12-state outbreak of Listeria monocytogenes that has hospitalized all 28 people affected and killed 2 since late May.
In an investigation notice posted late last week, the CDC said 16 of 18 people sickened (89%) reported eating meats sliced at deli counters (not packaged meats). The two deaths were reported from Illinois and New Jersey. Other affected states are Delaware, Georgia, Maryland, Massachusetts, Minnesota, Missouri, New York, North Carolina, Pennsylvania, and Virginia.
"This outbreak may not be limited to the states with known illnesses, and the true number of sick people is likely higher than the number reported," the notice said. "This is because some people recover without medical care and are not tested for Listeria."
The investigation is ongoing to determine the specific products that may have been contaminated. No products have been recalled.
At-risk people should avoid or heat sliced deli meats
The CDC recommends that people at high risk for severe Listeria infections (pregnant women, those aged 65 and older, and those with weakened immune systems) avoid eating deli-sliced meats or heat them to an internal temperature of 165°F or until steaming before consuming. Any containers and surfaces that may have touched the meats should be thoroughly cleaned with hot, soapy water.
Listeria spreads easily among deli equipment, surfaces, hands and food.
"Listeria spreads easily among deli equipment, surfaces, hands and food," the notice said. "Refrigeration does not kill Listeria, but reheating to a high enough temperature before eating will kill any germs that may be on these meats."
Infection usually causes fever, muscle aches, and fatigue but can also feature headache, stiff neck, confusion, balance problems, or seizures. Listeria can also lead to pregnancy loss or premature delivery in pregnant women, and life-threatening illness in newborns.
Symptoms typically begin within 2 weeks of eating contaminated food, but can start the same day or as late as 10 weeks later. Anyone with Listeria symptoms who recently ate sliced deli meats should call their healthcare provider, the CDC said.