Malaria infections during pregnancy are known to cause poor maternal and fetal outcomes and in Africa are thought to cause as many as 50,000 maternal deaths and 200,000 stillbirths each year. Tools such as bed nets and intermittent therapy have been inadequate, but immunizing women before pregnancy looks promising as a new strategy, researchers reported yesterday in The Lancet Infectious Diseases.
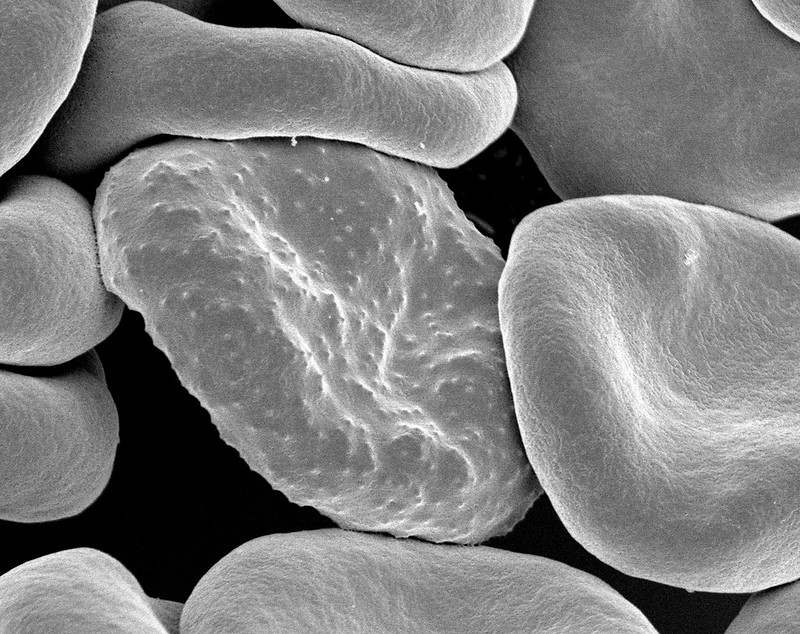
Researchers from the National Institutes of Health and their partners in Mali tested the strategy using PfSPZ, an investigational attenuated vaccine based on Plasmodium falciparum sporozoites made by Sanaria, based in Rockville, Maryland. Earlier clinical trials in Africa had found that the vaccine was safe and effective.
In Mali, researchers enrolled 300 women who planned on getting pregnant in the coming year. Participants were categorized into three groups. Two received either a low or high dose of the vaccine, and the third got a normal-saline placebo vaccine.
Participants received three doses, each a month apart. Investigators monitored the women for two malaria seasons over nearly 2 years. The team also tracked women who were pregnant over that period and followed-up on the health of the newborns through the first birthday.
Durable protection across 2 years
The vaccine was safe for both women and their babies. In the first year of the trial, 55 women became pregnant within 6 weeks of the third vaccine dose. Vaccine efficacy was 65% in those who received the lower dose and 86% in participants who got the higher dose. Of 155 women who became pregnant in both study years, efficacy was 57% for the lower dose and 49% for the higher dose.
In the next steps, the group will examine the safety of the PfSPZ vaccine during pregnancy and do a larger study on its preconception use.
In a related editorial in the same issue, Stephanie Yanow, PhD, and Daniel Ferrer Vinals, PhD, a cell biologist and chemical biologist, respectively, at the University of Alberta, wrote that the vaccine showed durable protection over 2 years without boosting, unlike other malaria vaccines. They said the preconception trial builds a good framework for assessing the vaccine in pregnant women, who are often excluded from trials.














