An analysis of urinary tract infection (UTI) isolates from East African countries found that roughly half were multidrug-resistant (MDR), researchers reported last week in JAC-Antimicrobial Resistance.
For the study, researchers recruited children and adults with UTI-like symptoms from healthcare facilities in Tanzania, Kenya, and Uganda and collected urine samples for microbiologic analysis, including antimicrobial susceptibility testing. MDR bacteria were defined as isolates resistant to at least one agent in three or more classes of antibiotic agents.
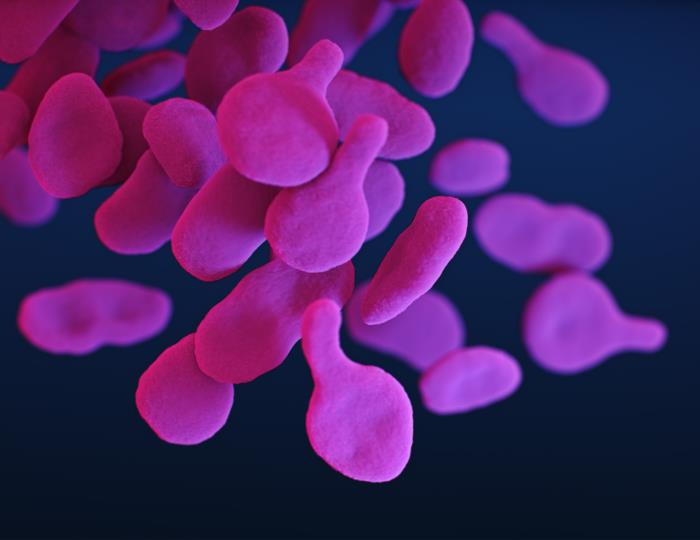
Of the 7,583 patients with symptomatic UTIs (3,852 from Tanzania, 1,903 from Kenya, 1,828 from Uganda), 2,653 (35.0%) had a microbiologically confirmed UTI. The predominant bacteria were Escherichia coli (37.0%), Staphylococcus (26.3%), Klebsiella (5.8%), and Enterococcus (5.5%). Of the 2,266 isolates submitted for antimicrobial susceptibility testing, 1,153 (50.9%) were categorized as MDR.
Findings fill 'crucial data gap'
MDR rates were 60.9% in Tanzania, 57.5% in Uganda, and 36.9% in Kenya. By pathogen, Staphylococcus had the highest MDR rate (60.9%), followed by E coli (52.2%), Klebsiella (50.6%), Enterococcus (38.1%), and other Enterobacterales (31.2%). The rate of MDR bacteria was much higher in inpatients than outpatients. The analysis also found "severely high" levels of resistance across pathogens to first-line antibiotics for UTIs.
The study authors say the findings fill a crucial data gap and should be used to inform guidelines for empiric antibiotic treatment of UTIs in East Africa.
They concluded, "More broadly, we emphasize the need for urgent investment in routine AMR surveillance programmes, expansion of diagnostic laboratory capacities and diagnostic algorithms to facilitate antimicrobial stewardship and call for greater commitment from policymakers to counter the threat of AMR."