Pharmaceutical company Merck last week announced positive topline results from two phase 3 trials of its investigational 21-valent pneumococcal vaccine.
The vaccine, V116, covers the 21 serotypes of Streptococcus pneumoniae that are responsible for 85% of invasive pneumococcal disease in adults ages 65 years and older and includes 8 serotypes that represent adult pneumococcal disease and are not currently covered by pneumococcal vaccines. If approved, it would be the first pneumococcal conjugate vaccine specifically designed for adults.
In the STRIDE-3 trial, V116 demonstrated statistically significant immune responses 30 days post-vaccination when compared with the pneumococcal 20-valent conjugate vaccine (PCV20) in vaccine-naïve adults for serotypes common to both vaccines. In the STRIDE-6 trial, which evaluated the safety, tolerability, and immunogenicity of V116 in adults aged 50 and older who had received pneumococcal vaccination at least one year before enrollment, the vaccine demonstrated immunogenicity for all 21 serotypes. Both studies showed V116 had a safety profile that was comparable to the comparator vaccines (PCV13, PCV15, PCV20, and PPSV23).
Could represent an additional weapon
"Despite the availability of current pneumococcal conjugate vaccines, many adults remain vulnerable to pneumococcal disease, especially those who are older," Eliav Barr, MD, senior vice president, head of global clinical development, and chief medical officer at Merck Research Laboratories, said in a company press release. "These results support the potential for V116 to become an important new preventative option for adults, regardless of prior pneumococcal vaccination status, by expanding coverage to include eight serotypes not currently included in any licensed vaccine."
Despite the availability of current pneumococcal conjugate vaccines, many adults remain vulnerable to pneumococcal disease, especially those who are older.
Merck says it will make the trial results available to the scientific community in the near future. Four other phase 3 trials of V116 are still ongoing.
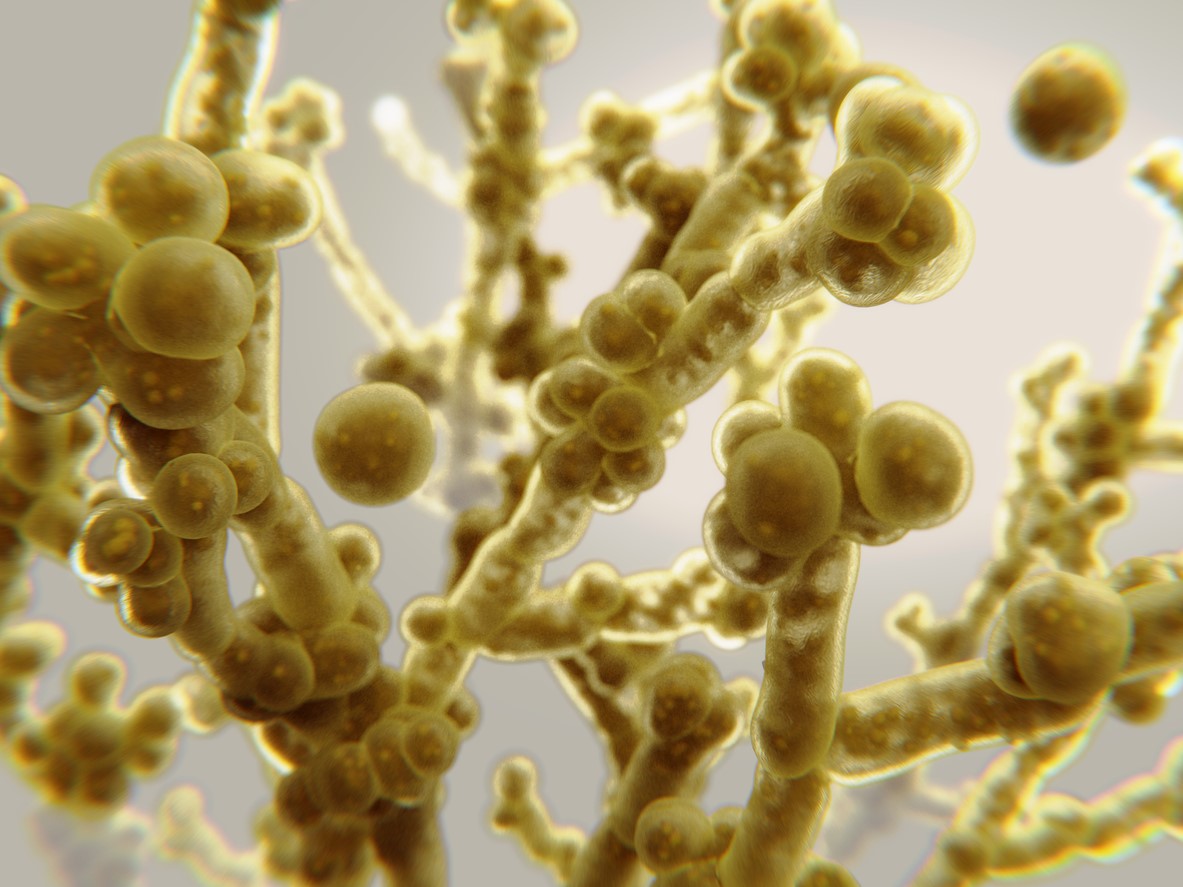 Testing by a team of researchers with the Louis Stokes Cleveland VA Medical Center indicates that sporicidal disinfectants are more effective against the multidrug-resistant fungal pathogen Candida auris than quaternary-ammonium disinfectants, according to a study published today in Infection Control & Hospital Epidemiology.
Testing by a team of researchers with the Louis Stokes Cleveland VA Medical Center indicates that sporicidal disinfectants are more effective against the multidrug-resistant fungal pathogen Candida auris than quaternary-ammonium disinfectants, according to a study published today in Infection Control & Hospital Epidemiology. The risk of flu-related intensive care unit (ICU) admission was sevenfold higher in lower middle-income countries (LMICs) than in high-income countries (HICs), according to an
The risk of flu-related intensive care unit (ICU) admission was sevenfold higher in lower middle-income countries (LMICs) than in high-income countries (HICs), according to an 













