
The rate of invasive pneumococcal disease (IPD) in children plummeted 72% from 2002 to 2021 and continued to fall after the 7-valent (7-strain) pneumococcal conjugate vaccine (PCV7) was replaced by the 13-valent version (PCV13), a Yale University–led team reports today in Pediatrics.
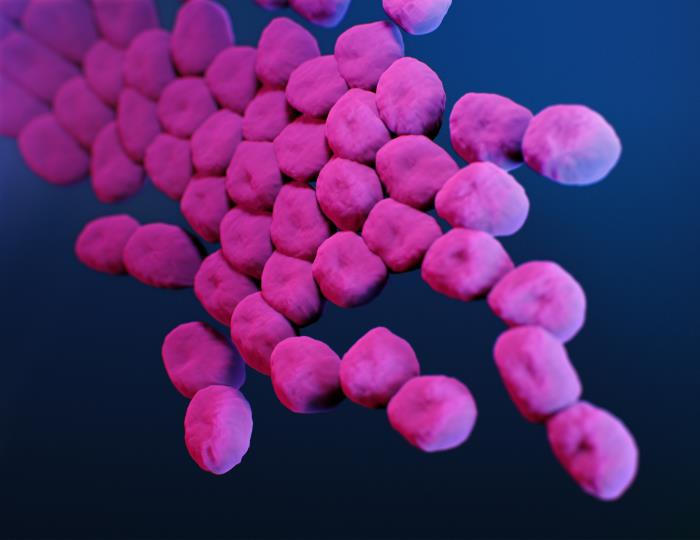
The study analyzed data on IPD among children younger than 18 years from a Massachusetts surveillance system. The team serotyped Streptococcus pneumoniae isolates from normally sterile sites and evaluated them for antimicrobial susceptibility.
PCV7 was rolled out in the United States in 2000 and was replaced by PCV13 in 2010. Vaccine uptake in Massachusetts among children younger than 3 years with three or more doses is 92%, and receipt of at least four doses is 81% to 91%.
The researchers defined protective vaccination as receipt of two or more doses for children younger than 1 year, three doses in the first year of life, or one dose after 1 year.
IPD dipped to 1.6 per 100,000 amid pandemic
In all, 1,347 IPD cases were identified. Rates in children fell 72% (incidence rate ratio, 0.28) and continued to decline after replacement of PCV7 with PCV13 (incidence rate ratio, 0.25 in the late PCV7 vs the late PCV13 era).
In the COVID-19 pandemic years 2020 to 2021, IPD incidence dipped to a low of 1.6 per 100,000 children. In the PCV13 era, 30.3% of infected children older than 5 years had at least one underlying medical condition.
Robust ongoing surveillance networks are critical for identifying emerging serotypes and development of next-generation vaccine formulations.
Serotypes 19A and 7F made up 48.9% of infections before replacement with PCV13. Serotype 3 (8.6%) and non-PCV13 serotypes 15B/C (10.8%), 33F (8.0%), 23B (0.8%), and 35B (4.7%) caused 37.8% of cases in the PCV13 era. Nonsusceptibility to penicillin continued to fall (9.8% vs 5.3% in the pre-/late PCV13 era) but has become more common among non-PCV13 serotypes than vaccine serotypes (14.8% vs 1.4%).
"Nonvaccine serotypes continue to emerge under vaccine-selective and antibiotic-selective pressures, limiting overall vaccine effectiveness against pneumococcal disease," the authors wrote. "Robust ongoing surveillance networks are critical for identifying emerging serotypes and development of next-generation vaccine formulations."



.jpg)














