A study today in the New England Journal of Medicine discusses a phase 3 randomized, controlled trial of GSK's respiratory syncytial virus (RSV) vaccine in pregnant women that was stopped early owing to an increased risk of preterm birth.
Researchers from GSK and the Duke University School of Medicine assessed the efficacy and safety of the RSVPreF3-Mat vaccine in 5,328 pregnant women aged 18 to 49 years and 5,233 infants from November 2020 to February 2022, when enrollment and vaccination were stopped after a link to preterm birth was noted.
The trial was conducted at sites in 24 countries on six continents, with roughly half of the participants in the vaccine and control groups from low- and middle-income countries (LMICs). The team randomly assigned participants in a 2:1 ratio to receive either RSVPreF3-Mat or a placebo between 24 and 34 weeks' gestation. In total, 3,426 infants whose mothers received the vaccine and 1,711 infants whose mothers received placebo were followed from birth to 6 months.
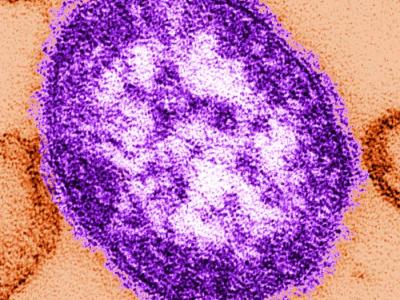
RSV is a leading cause of lower respiratory tract disease in children and can be particularly severe in infants younger than 6 months old, especially those in LMICs.
In July 2023, the US Food and Drug Administration (FDA) approved nirsevimab (brand name, Beyfortus), a long-acting monoclonal antibody, for RSV prevention in infants. In August 2023, the FDA approved the first RSV vaccine based on the RSV prefusion F protein (Pfizer's bivalent [two-strain] RSVPreF; brand name, Abryvso) for pregnant women from 32 to 36 weeks' gestation; it isn't given before 32 weeks' gestation because of a potential risk of preterm birth. Abryvso is also approved for use in people aged 60 years and older.
RSVPreF3-Mat is a monovalent, or single-strain, vaccine.
Risk of preterm birth 37% higher in vaccine group
Sixteen and 24 infants in the vaccine and placebo groups, respectively, had medically assessed RSV-associated lower respiratory tract disease (vaccine effectiveness [VE], 65.5%; 95% credible interval [CrI], 37.5% to 82.0%), and 8 and 14, respectively, had severe RSV (VE, 69.0%; 95% CrI, 33.0% to 87.6%).
Of the 3,494 infants in the vaccine group, 237 (6.8%) were born early, compared with 86 of 1,739 (4.9%) in the placebo group (relative risk [RR], 1.37). Also 13 of 3,494 (0.4%) and 3 of 1,739 (0.2%), respectively, died (RR, 2.16), an imbalance seen primarily in LMICs (RR, 1.56 vs 1.04 in high-income countries). The authors said the disparity was likely at least partly attributable to the greater percentage of preterm births in the vaccine group.
The results of this trial, in which enrollment was stopped early because of safety concerns, suggest that the risks of any and severe medically assessed RSV-associated lower respiratory tract disease among infants were lower with the candidate maternal RSV vaccine than with placebo but that the risk of preterm birth was higher with the candidate vaccine.
In other words, for every 54 infants born to vaccine recipients, 1 additional preterm birth occurred, with the time from vaccination to preterm birth varying from weeks to months. Among the infants born early, very preterm birth (28 to 32 weeks' gestation) or extremely preterm birth (less than 28 weeks' gestation) occurred in 13 of 237 (5.5%) in the vaccine group and 2 of 86 (2.3%) in the placebo group. No other safety signals were reported.
"The results of this trial, in which enrollment was stopped early because of safety concerns, suggest that the risks of any and severe medically assessed RSV-associated lower respiratory tract disease among infants were lower with the candidate maternal RSV vaccine than with placebo but that the risk of preterm birth was higher with the candidate vaccine," the researchers wrote.
Mechanism of increased risk unknown
In a related commentary, Sonja Rasmussen, MD, of Johns Hopkins University, and Denise Jamieson, MD, MPH, of the University of Iowa, noted that it's unknown whether the safety signal in the RSVPreF3-Mat trial was real or a chance event.
Given the findings of the present trial and the modest imbalance in the incidence of preterm birth in the phase 3 trial of the bivalent vaccine [Abryvso], postmarketing surveillance of the bivalent vaccine is warranted.
"Despite many post hoc analyses, the authors were unable to identify a mechanism by which the receipt of RSVPreF3-Mat might have increased the risk of preterm birth," they wrote. "However, given the findings of the present trial and the modest imbalance in the incidence of preterm birth in the phase 3 trial of the bivalent vaccine [Abryvso], postmarketing surveillance of the bivalent vaccine is warranted."
"Even if there is a true association between the receipt of the bivalent vaccine and preterm birth, it is essential to weigh this small risk against the proven benefits of maternal RSV vaccination," they added. "Moreover, any potential risk of preterm birth associated with the receipt of the bivalent vaccine is reduced by the administration of the vaccine at 32 weeks or more of gestation."