In today's New England Journal of Medicine, researchers describe the phase 3 trial results of the newly approved modified vaccinia Ankara vaccine (MVA) and said the vaccine is safe and likely effective against smallpox, which is caused by the variola virus.
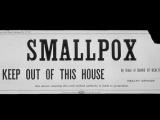
Though smallpox was declared eradicated in 1980, the usefulness of a smallpox vaccine has been touted as a way to protect against the variola virus if used as a bioweapon, or if the virus is reintroduced into a naive population through a lab accident. A smallpox vaccine could also protect against other orthopoxviruses, such as monkeypox.
Toe to toe with ACAM2000
To conduct the study, researchers vaccinated 208 US soldiers deployed in South Korea with two doses of MVA before one dose of the established replicating-vaccinia vaccine ACAM2000, and compared that group to an ACAM2000-only control group of 213.
ACAM2000, which contains live vaccinia virus, was approved for use by the US Food and Drug Administration (FDA) in 2007.
The goal was to see if MVA was non-inferior to ACAM2000 in producing antibodies against vaccinia, a virus similar to smallpox, and if the group first dosed with MVA developed smaller lesions than the ACAM2000 group. In previous studies, MVA did not cause cutaneous reactions because of a lack of replication in human cells, the authors said.
MVA vaccination did elicit a robust immune response, with a mean titer of neutralizing antibodies of 153.5 at week 6, as compared with 79.3 at week 4 with ACAM2000 (a ratio of 1.94 [95% confidence interval, 1.56 to 2.40]. The geometric mean titer of neutralizing antibodies induced by a single MVA dose (16.2) was equal to that induced by ACAM2000 at 2 weeks, and 90.8% of MVA recipients had seroconversion, compared with 91.8% in the ACAM2000 group.
The MVA group also produced much fewer and smaller blisters, or "takes," than those seen in the ACAM2000-only group.
"Previous MVA vaccination prevented formation of a full major cutaneous reaction in the majority of participants (77.0%) after subsequent ACAM2000 vaccination, as compared with a rate of full major cutaneous reaction of 92.5% after ACAM2000 alone," the authors wrote.
MVA as an antigen-delivery platform
The FDA approved MVA, under the trade name Jynneos, on Sep 24 to prevent both smallpox and monkeypox. The approval made MVA the first vaccine approved for monkeypox, and the first non-replicating vaccine approved against smallpox, which means the modified vaccinia viruses it contains cannot reproduce in human cells.
"Although naturally occurring smallpox disease is no longer a global threat, the intentional release of this highly contagious virus could have a devastating effect," Peter Marks, MD, PhD, director of the FDA's Center for Biologics Evaluation and Research, said at the time of the approval.
Jynneos was placed in the Strategic National Stockpile and is available for people at risk for monkeypox or smallpox.
In an accompanying New England Journal of Medicine commentary, Lindsey Baden, MD, of Boston's Brigham and Women's Hospital, and Inger Damon, MD, PhD, director of the Centers for Disease Control and Prevention's Division of High-Consequence Pathogens and Pathology, write about the challenge of creating and testing a vaccine for a disease that no longer exists in nature.
"How are new therapies to be developed for a disease that no longer exists? Although the established vaccine for smallpox, which currently consists of vaccinia virus, is highly effective, it has considerable limitations, including a risk of disseminated local and systemic infection and, in very rare cases, death," they write.
The encouraging data from the phase 3 trial will likely encourage more researchers to look at MVA as an antigen-delivery platform.
"MVA is being developed not only as a primary immunogen but also as a delivery system for genes and gene products to combat various other conditions, including prostate cancer, HIV-1 infection, and Ebola virus disease," Baden and Damon write.
"We must ensure that the immune markers and biomarkers developed clearly correlate with the outcome of interest—attenuation or prevention of human disease."
See also:
Nov 14 N Engl J Med study
Nov 14 N Engl J Med commentary
Sep 24 FDA press release