Nearly 80% of COVID-19 patients in 28 countries received early empiric antibiotics during the first year and a half of the pandemic, US and Turkish researchers reported yesterday in the International Journal of Infectious Diseases.
Using data from the Society of Critical Care Medicine Discovery VIRUS International COVID-19 Registry, the researchers looked at the rate of coinfections at admission and the rate and factors associated with early empiric antibiotic use in COVID-19 patients from January 2020 to October 2021. They focused on antibiotics administered within the first 3 days of hospitalization, particularly azithromycin, which was thought early on to have a beneficial effect when combined with hydroxychloroquine. After exclusions, 7,830 patients were included in the analysis.
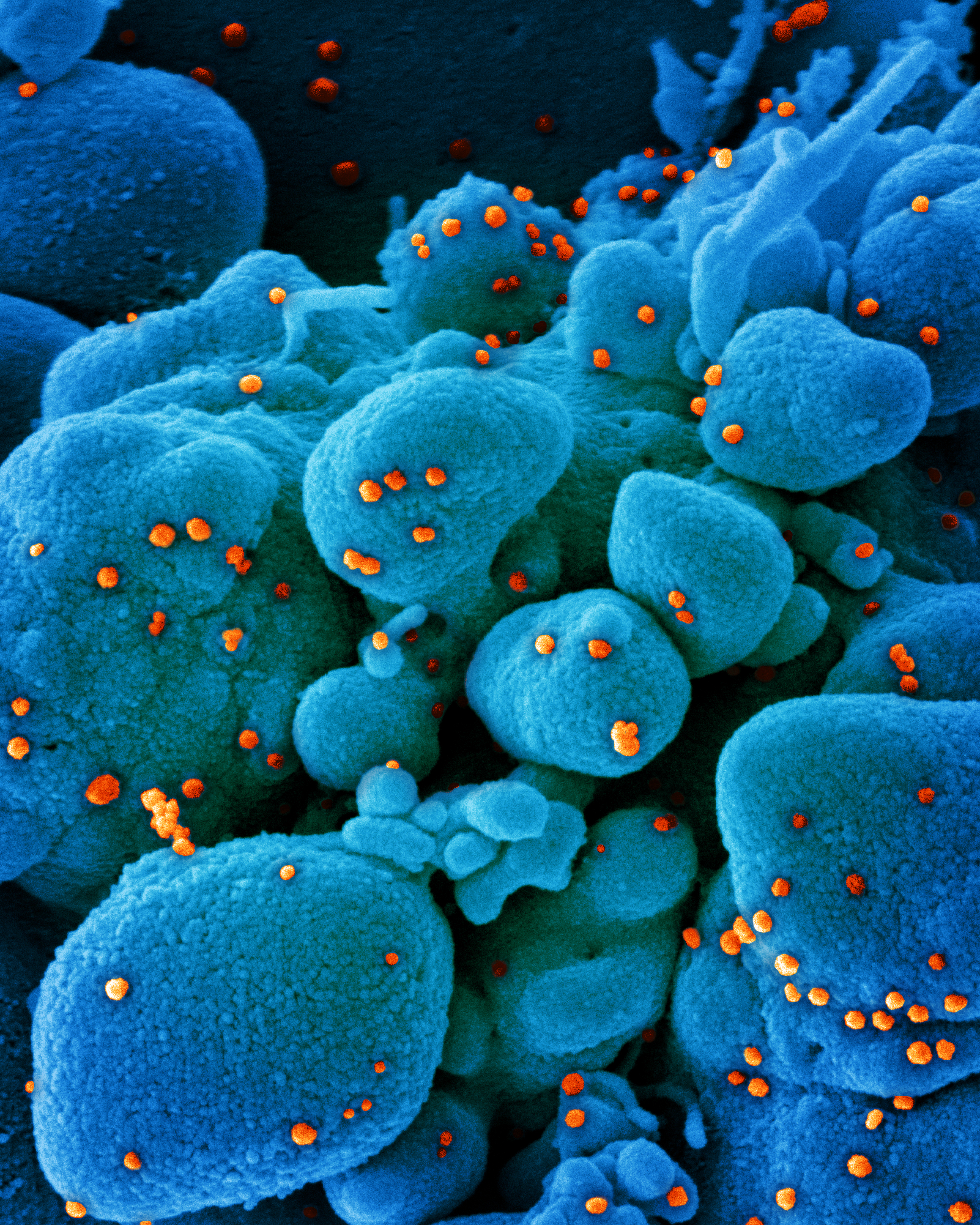
The vast majority of patients (79.4%) received early empiric antibiotic treatment, with 40.2% receiving a combination of azithromycin and another antibiotic. The proportion of patients receiving early empiric antibiotic treatment fell from 84.4% in the first quarter of 2020 (January to March 2020) to 65.2% in April-June 2021. Beta-lactams, specifically ceftriaxone, were the most commonly used non-azithromycin antibiotic. Of the 7,830 patients, 5.8% had culture-proven community-acquired respiratory coinfections at the onset of hospitalization, with Staphylococcus aureus the most common (24%) pathogen isolated.
Decreasing trend over time
Multivariate analysis revealed that patients from Southeast Asia had the highest odds (odds ratio [OR], 77.8; 95% confidence interval [CI], 31.9 to 190.4) of receiving antibiotics compared with other regions. As the pandemic advanced, the OR of receiving any antibiotic treatment declined from 5.9 (95% CI, 2.7 to 13.0) to 4.1 (95% CI, 1.9 to 8.9). Diabetes, fever, and difficulty breathing were independently associated with antibiotic use.
The study authors say the decline in the frequency of early empiric antibiotic treatment over the study period could be attributed to antibiotic stewardship efforts, along with faster polymerase chain reaction test turnaround times and the failure of hydroxychloroquine-azithromycin treatment to show any benefit in COVID patients.
"Our study provides worldwide goals for antibiotic stewardship programs in COVID-19 setting as well as for future viral pandemics," they wrote. "Further research is needed to better understand the factors that influence antibiotic use during the pandemic and to optimize treatment for patients with COVID-19."