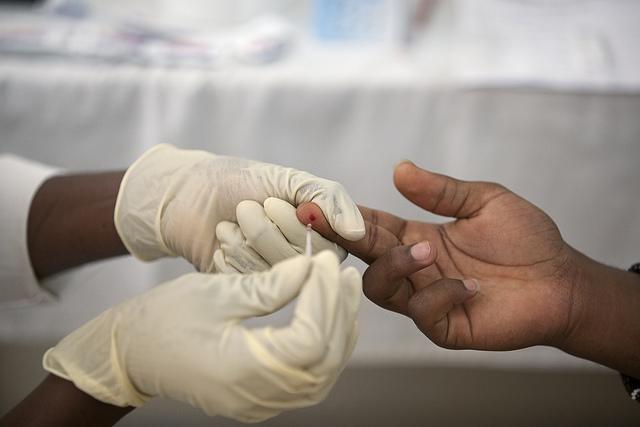
Rapid diagnostic tests (RDTs) for malaria have helped reduce overprescribing of antimalarial drugs in parts of the world where the parasitic disease is endemic and healthcare resources are scarce. That's a good thing, given that development of resistance to antimalarials is one of the greatest threats to malaria control.
But since malaria-endemic countries in Africa and Asia started using the small devices—which can quickly detect the presence of specific antigens produced by malaria parasites from a pinprick of blood—there has been concern among some public health professionals about the potential for an unintended consequence: increased use of antibiotics to treat patients who've tested negative for malaria.
That's because, in settings with little healthcare infrastructure, treating febrile illness often amounts to "educated guesswork," according to the authors of a new study in the British Medical Journal (BMJ).
To determine if this concern has been borne out, an international research team led by Heidi Hopkins, MD, a professor of malaria and diagnostics at the London School of Hygiene and Tropical Medicine, reviewed nine observational and randomized studies in Africa and Asia. The papers compared antibiotic prescribing in trial groups who had received RDTs with control groups, and in patients with negative test results compared with those who tested positive for malaria.
The results of that analysis, Hopkins told CIDRAP News, suggest that "these concerns are well-founded in many settings."
Antibiotic prescriptions climb 21%
The studies, conducted from 2007 through 2013 in a mix of urban and rural settings in Afghanistan, Cameroon, Ghana, Nigeria, Tanzania, and Uganda, included more than 500,000 children and adults with acute febrile illness. The analysis of the studies found that antibiotics were prescribed to 53% of patients in control groups and 59% of patients in groups who had received RDTs. A meta-analysis of the studies showed that the risk of antibiotic prescription was 21% higher in places where RDTs were introduced.
When the researchers compared patients who had negative tests results with patients who tested positive, they found that antibiotics were prescribed to 69% of patients with a negative test results and 40% of those who tested positive for malaria. In most settings where the tests were used, patients with malaria-negative test results were more likely to receive the four most common antibiotic classes—penicillins, trimethoprim-sulfamethoxazole, tetracylines, and metronidazole—than those who tested positive.
Hopkins said that while she and her colleagues weren't surprised to find an increase in antibiotic use among patients who had undergone rapid diagnostic testing, the size of the increase stood out. "We expected to find only a marginal increase in antibiotic prescription for patients with negative malaria test results, but in many settings it appears to be significant," she said.
While these studies don't reveal whether the patients who tested negative for malaria actually had a bacterial infection, Hopkins said studies done in similar settings have shown that relatively few patients have infections that require antibiotics. "Based on those studies, we can estimate that just a small proportion of patients with fever are likely to need antibiotics—almost certainly fewer than the 69% who had negative malaria test results and who received antibiotics in our analysis.
"The challenge in any setting is to know which patients do, and don't, require antibiotics," she said.
Educated guesswork
The challenge for health workers treating patients with fever in tropical, low-resource settings is even greater. The lack of access to facilities that can confirm diagnoses and identify pathogens, Hopkins explained, means health workers often have to prescribe treatment without knowing the exact cause of illness. And many patients who present with fever expect to receive antibiotics.
But as Hopkins and her colleagues note in the study, case management guidelines for limited-resource settings do not recommend empirical antibiotics for non-severe febrile illness when the cause of the illness is unclear.
To address this shift toward overuse of antibiotics, Hopkins said further studies are needed to identify some of the reasons health workers prescribe antibiotics for patients who test negative for malaria. In addition, the treatable or preventable causes of non-malaria febrile illness need to be identified so that health workers don't have to rely on guesswork.
Hopkins also believes that the development of easy-to-use RDTs for other infectious diseases could improve treatment in low-resource settings. "Such tests should prove very useful in the future—but we should take advantage of lessons learned from malaria RDT implementation so that we can introduce new tests in a way that optimizes use of medicines and patient outcomes," she said.
See also:
Mar 29 BMJ study