A case report published today in Morbidity and Mortality Weekly Report highlights the role of the hospital water environment in the transmission of highly resistant, difficult-to-treat pathogens.
The report by researchers with the Centers for Disease Control and Prevention (CDC), Idaho Division of Public Health (IDPH), and Utah Public Health Laboratory (UPHL) describes the identification and investigation of carbapenemase-producing, carbapenem-resistant Pseudomonas aeruginosa (CP-CRPA) in two patients who stayed in the same room in an intensive care unit (ICU) in Idaho 4 months apart.
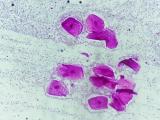
The opportunistic pathogen, which was ultimately traced to a sink in the shared room, persists in the hospital environment, where it can spread easily between patients and cause severe invasive infections,
Investigators target plumbing as the source
The pathogen was first identified by hospital staff on September 17, 2021, in the sputum of a woman who had received mechanical ventilation during 3 of 5 weeks of ICU hospitalization. Whole-genome sequencing by UPHL, which belongs to the CDC Antibiotic Resistance Laboratory Network, detected the imipenem metallo-beta-lactamase gene type 84 (blaIMP-84)—one of the less commonly reported carbapenemase genes—and characterized the isolate as belonging to multilocus sequence type 235 (ST235).
On January 25, 2022, CP-CRPA was isolated from a second patient who shared the same room while receiving mechanical ventilation for 4 weeks. Sequencing of the isolate by UPHL confirmed it also belonged to ST235 and carried the blaIMP-84 gene. But there was no evidence of person-to-person transmission.
Although no CP-CRPA was detected in the 16 patients who stayed in the room between the two patients, no patients were placed in the room after January 25, and IDPH officials visited the hospital in March 2022 to investigate the cluster and collect environmental samples.
Collaboration between health care facilities and public health agencies, including testing of CRPA isolates for carbapenemase genes and implementation of sink hygiene interventions, was critical in the identification of and response to this CP-CRPA cluster in a health care setting.
One area focused on by IPHL was the non-disposable parts of the ventilators, where pathogens like CRPA can reside if not properly cleaned. But based on consultation with the CDC, the investigators also examined the plumbing in the room, because P aeruginosa is known to form complex communities of bacteria known as biofilms, which thrive in warm, wet environments. Previous research, in fact, has found that CRPA is one of the most common carbapenem-resistant organisms found in the hospital water environment.
IPHL investigators collected water samples and swabs from two sinks and one toilet in the room. CP-CRPA was isolated from a toilet water sample and one of the sinks, and sequencing revealed the sink isolates were genetically similar to the isolates from the two patients.
Following this discovery, a disinfectant was added to the sink drain cleaning procedure, and sampling of the sinks and toilet in the room 13 days after the seventh disinfectant application found no CRPA. As of December 2022, no subsequent cases were detected.
"Collaboration between health care facilities and public health agencies, including testing of CRPA isolates for carbapenemase genes and implementation of sink hygiene interventions, was critical in the identification of and response to this CP-CRPA cluster in a health care setting," the authors wrote.