A systematic review and meta-analysis found that reactions to direct penicillin challenges in patients with penicillin allergy histories are infrequent, researchers reported today in JAMA Internal Medicine.

The review included 56 primary studies involving participants who underwent a direct penicillin challenge, which involves giving a patient with a low-risk penicillin allergy history a small oral dose of a penicillin without prior testing and then observing them for a possible reaction. The procedure is viewed as a more feasible and less costly method for confirming a penicillin allergy than skin testing, but the perceived risk of reaction remains a barrier. More than 95% of patients with a penicillin allergy label are not truly allergic.
Among the 9,225 participants in the studies, 438 experienced reactions to a direct penicillin challenge, corresponding to an overall meta-analytic frequency of 3.5% (95% credible interval [CrI], 2.5% to 4.6%), with a frequency of 2.2% (95% CrI, 1.2% to 3.2%) for children and 6.6% (95% CrI, 4.6% to 9.5%) for adults.
A higher risk of reaction was found in studies performed in children (odds ratio [OR], 3.37; 95% CrI, 1.98 to 5.98), in outpatients (OR, 2.19; 95% CrI, 1.08 to 4.75), and those performed using a graded (OR, 3.25; 95% CrI, 1.50 to 7.06) or prolonged (OR, 5.45; 95% CrI, 2.38 to 13.28) challenge. Studies performed in North America had a lower risk of reaction (OR, 0.36; 95% CrI, 0.20 to 0.61). Only five severe reactions occurred across included studies.
Results could boost penicillin allergy delabeling
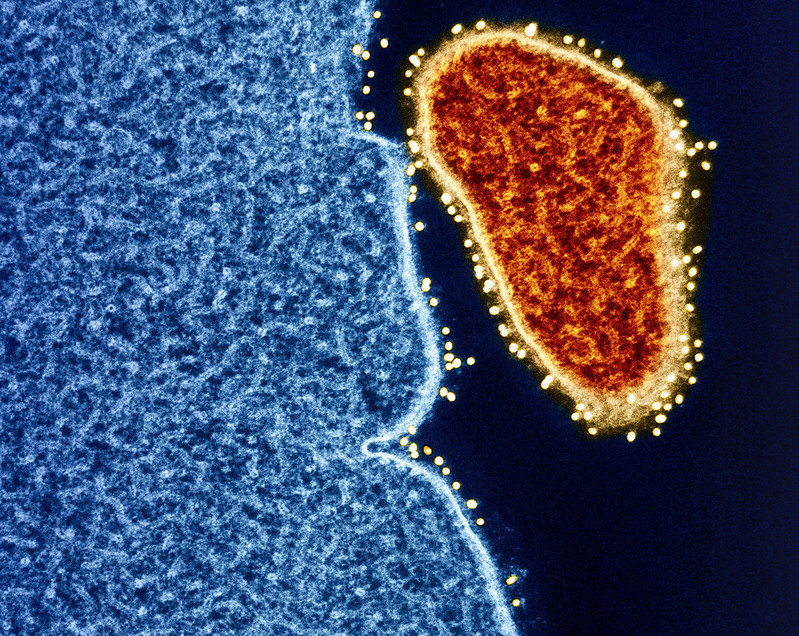
The study authors say the findings are important because patients with penicillin allergies are more likely to be treated with second-line antibiotics, which may lead to longer hospital stays and higher healthcare costs, and the use of broad-spectrum second-line agents has been associated with the development of antimicrobial resistance. They hope that more use of direct penicillin challenges could expand penicillin allergy delabeling efforts.
"Considering that up to 50% of inpatients are treated with antibiotics, it is crucial to increase penicillin allergy assessments and delabel those without the allergy to prevent the adverse outcomes associated with deferring first-line antibiotics," they wrote.