Chronic wasting disease (CWD) surveillance in central and north central Nebraska netted 31 positive cases in deer, including those in three new counties, during the November firearm season, Nebraska Game and Parks (NGP) said yesterday in a news release.
Hunters supplied 603 deer samples to check stations in the Sandhills, Keya Paha, Calamus East, Calamus West, and Loup West deer management units. For the first time, CWD was found in Rock, Blaine, and Thomas counties, all in the north-central part of the state.
Hunter caution urged
NGP conducts surveillance in five to seven deer management units each year, rotating to a different area each time. CWD was first found in Nebraska in 2000 in Kimball County in the west, which borders both Wyoming and Colorado. NGP has tested more than 57,000 deer and 400 elk since 1997, with 1,269 deer and 19 elk in 57 counties testing positive.
CWD prions, the infectious proteins that transmit the disease, can remain viable for months or even years in the soil.
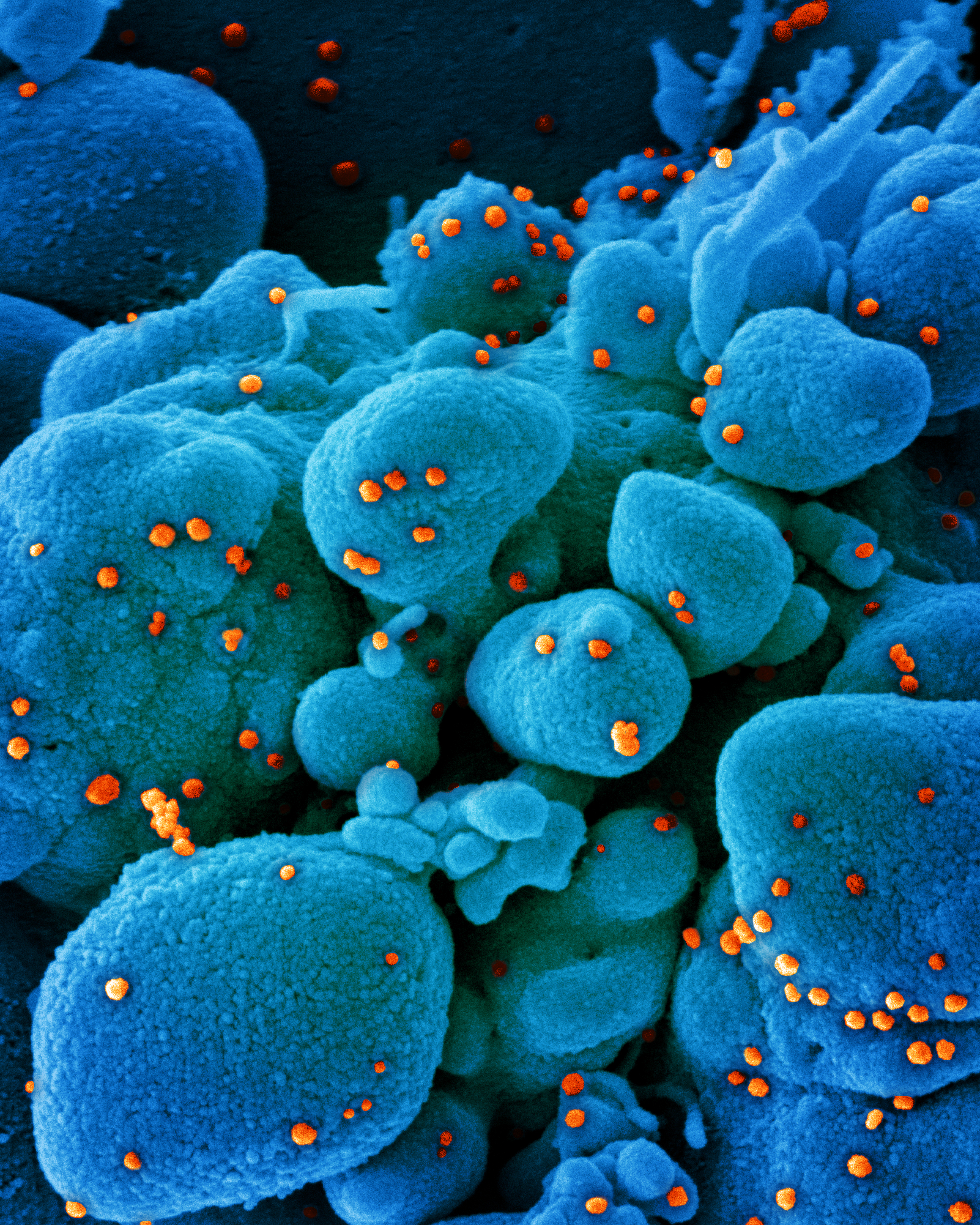
CWD is a fatal neurodegenerative disease caused by infectious misfolded proteins called prions. While CWD is not yet known to infect humans, the Centers for Disease Control and Prevention advises hunters to not consume meat from any animal that is obviously ill or tests positive for the disease.
"CWD prions, the infectious proteins that transmit the disease, can remain viable for months or even years in the soil," NGP said in the news release. "Hunters should field dress animals at the place of kill, avoid spreading spinal cord or brain tissue to meat, and to dispose of the head (brain), spinal column, and other bones at a licensed landfill."