Editor's note: Today's commentary was submitted to CIDRAP by the authors, who are national experts on respiratory protection and infectious disease transmission. In September they published a commentary on optimal respiratory protection for Ebola, and in May they published a similar commentary on MERS-CoV. Dr Jones is an Assistant Professor and Dr Brosseau is a Professor in the School of Public Health, Division of Environmental and Occupational Health Sciences, at the University of Illinois at Chicago. Submitted commentaries do not necessarily represent the scientific position of CIDRAP.
Authors' disclaimer: This commentary reflects the personal opinions of the authors. It does not represent the opinion of the University of Illinois at Chicago or any other organization. The authors have not received any compensation for the preparation of this commentary or any associated public statements. The authors do not endorse any specific manufacturer or brand of personal protective equipment (PPE) and have no direct or indirect financial interest in the use of a specific brand of PPE.
On Oct 20, the US Centers for Disease Control and Prevention (CDC) released updated guidelines for the protection of healthcare workers caring for patients with Ebola virus disease (EVD).1 The CDC guidance states, "In healthcare settings, Ebola is spread through direct contact (e.g., through broken skin or through mucous membranes of the eyes, nose, or mouth) with blood or body fluids of a person who is sick with Ebola or with objects (e.g., needles, syringes) that have been contaminated with the virus."
In a previous commentary, we discussed why direct contact may not be the only mode of EVD transmission, particularly in healthcare settings. An Institute of Medicine report released last week underscores the importance of conducting studies to better understand all modes of EVD transmission, including by aerosols.2 We describe here a new paradigm of disease transmission that includes direct contact, indirect contact, and aerosol transmission. We also discuss evidence that supports Ebola transmission by all of these modes in patient care settings—and highlight why the CDC guidance might oversimplify transmission and underestimate risks.
The traditional disease transmission paradigm for healthcare settings
As we understand the traditional disease transmission paradigm for healthcare settings, three primary modes of transmission exist: contact, droplet, and airborne. Each mode of transmission is associated with a suite of infection control practices.
Contact transmission is described by the Healthcare Infection Control Practices Advisory Committee (HICPAC) as3:
- Direct contact transmission, which "occurs when microorganisms are transferred from one infected person to another person without a contaminated intermediate object or person," or
- Indirect contact transmission, which "involves the transfer of an infectious agent through a contaminated intermediate object or person."
An example of direct contact transmission is the direct entry of blood or body fluids containing microorganisms into a healthcare worker's body through breaks in her skin, such as when she touches a patient's wound. In indirect contact transmission, the body fluid containing the microorganism contaminates an object, such as a piece of medical equipment, and the microorganism transfers into the healthcare worker's body through breaks in his skin when he handles the object.
Droplet transmission is described by HICPAC as a form of direct contact transmission in which "respiratory droplets carrying infectious pathogens transmit infection when they travel directly from the respiratory tract of the infectious individual to susceptible mucosal surfaces of the recipient, generally over short distances, necessitating facial protection." These droplets are considered "propelled" from the infectious person. An infectious patient may emit droplets during coughing, sneezing, and talking and through medical procedures like suctioning, endotracheal intubation, cough induction by chest physical therapy, and cardiopulmonary resuscitation.
Airborne transmission is defined by HICPAC as resulting from the inhalation of small respirable particles that "remain infective over time and distance" and "can be dispersed over long distances by air currents." This description seems to imply that transmission will occur only if the person being infected is not face-to-face with an infectious individual. In some cases, this mode of transmission has been interpreted to mean that infection occurs only outside the space occupied by the infectious person.
HICPAC uncertainty about traditional modes of transmission
HICPAC describes some uncertainty about droplet transmission with respect to safe distances between an infectious patient and a healthcare worker, and the particle size of droplets.
Historically, droplet transmission risk was considered to be limited to workers within 3 feet of an infectious patient.3 HICPAC accurately notes, "It is likely that the distance droplets travel depends on the velocity and mechanism by which respiratory droplets are propelled from the source, the density of respiratory secretions, environmental factors such as temperature and humidity, and the ability of the pathogen to maintain infectivity over that distance," and recognizes that epidemiologic evidence from SARS suggests the distance could extend beyond 6 feet. However, HICPAC explains that even if we don't know the exact distance for droplet transmission, when compared with airborne pathogens, droplets do not transmit infection over long distances. The term "long distances" is not defined.
According to HICPAC, "Droplets traditionally have been defined as being >5 micrometers [mcm] in size." In contrast, droplet nuclei are 5 mcm or smaller, and are considered to be droplets that have partially evaporated. Droplet nuclei are considered responsible for airborne transmission, but it is well known that particles with diameter larger than 5 mcm can remain suspended in air and can be inhaled. In addition, it is well known that particles smaller than 5 mcm in diameter are emitted in activities considered to generate respiratory droplets, like coughs, and can project through the air onto mucosal surfaces.
Turning to limitations of the definition of airborne transmission, HICPAC notes that selected respiratory viruses (influenza and rhinovirus) and gastrointestinal viruses (norovirus and rotavirus) may be transmitted by small-particle aerosols, despite their primary classification as droplet- and contact-transmissible agents, respectively. This is the first time the term "aerosol" is used by HICPAC, but it is neither defined nor explained in comparison to droplets or droplet nuclei.
A new approach in healthcare settings: aerosol transmission
Central to HICPAC uncertainties are their artificial distinctions about particle size and transport distance. To resolve these conflicts, we propose an aerosol transmission route to replace droplet and airborne transmission. An aerosol is a collection of particles suspended in the air; these particles may contain infectious microorganisms if the aerosol is emitted from an infectious patient.
Aerosols generated by human biological processes and medical procedures contain microorganism-laden particles that vary in size by several orders of magnitude, including particles that would be classified as droplets and as droplet nuclei, and may be emitted with force. Thus, if a worker is near the aerosol source, the worker may inhale particles and may have particles project onto his or her mucosal surfaces.
Under the traditional paradigm, a worker near an infectious patient who is emitting aerosol would be considered at risk of droplet transmission and offered personal protective equipment (PPE), such as a surgical mask, face shield, or goggles, that prevents the projection of microorganism-laden particles onto the mucosal membranes but does not prevent particle inhalation. Thus, healthcare workers remain at risk of exposure to inhaled microorganism-laden particles when near an infectious patient.
Understanding aerosol transmission
Consider the cough as a prototypical process of aerosol emission. A cough aerosol contains particles that range in size over several orders of magnitude.4 The fate of this aerosol is complex and dynamic.
Like many particles of body fluids, cough particles contain liquid and will evaporate to smaller particles, losing about 50% of their diameter within a second of release.5 There will still be a wide range of particle sizes present in the aerosol, but the particles will be smaller than when they were first generated.
In addition to changing size, some particles may project onto surfaces, some settle onto surfaces due to gravity, and others remain suspended in the air for long periods, with larger particles settling faster than smaller ones. Particles are dispersed throughout a room by air movements; smaller particles will also undergo diffusion by interaction with air molecules. A person standing near the cough will inhale particles of all sizes, which deposit in different patterns within the respiratory tract, depending on their size.
Figures 1, 2, and 3 illustrate these processes. Figure 1 represents the initial aerosol generation from an infected person. At the point of generation (time = 0), the particles are close together, so the concentration near the source is high. Figures 2 (time = 1) and 3 (time = 2) illustrate how, as time passes, larger particles settle more rapidly from the room air and do not travel far from the source. Smaller particles, however, eventually become distributed throughout the air with a lower concentration than at the initial point of generation.
Figure 1. When an aerosol is initially emitted (time = 0), the particles are clustered near the source at location A. A person near the source (location B) may receive large-particle spray and inhale particles of all sizes.
Figures: Absolute Science Illustration

Figure 2. After some time (time = 1), the particles begin to disperse and larger particles begin to settle from the air. Person B will continue to inhale particles of all sizes.

Figure 3. After more time (time = 2), the small particles are uniformly dispersed and more of the larger particles have settled from the air. Persons B and C will inhale particles that are generally smaller, have a smaller size range, and are at a lower concentration than at time = 0.

At the time of aerosol emission (time = 0, figure 1) a person such as a healthcare worker standing at point B will experience aerosol exposure, including the spray of body fluids onto the skin, face, eyes, mouth, nose, etc., and will inhale particles of all sizes suspended in air. At time = 1, the person located at point C will not have any exposure (figure 2). But at time = 2, the people at points B and C will inhale suspended particles (figure 3).
Understanding inhalation of aerosols
Microorganism-laden particles suspended in air (aerosols) may be inhaled, deposited in the respiratory tract, and reach cells in which infection can begin. This occurs even for microorganisms that do not cause respiratory infections. For example, epidemiologic evidence suggests that norovirus can initiate gastrointestinal infection following inhalation and subsequent ingestion. Large numbers of people have been infected in a norovirus outbreak even when they were not within 10 feet of the infectious person who vomited.6,7 These observations also suggest that norovirus is capable of remaining viable in the environment for a relatively long period, is highly infectious, or both.
Figure 4 shows how the percent of aerosol particles that are inhaled and deposited varies among the different regions of the respiratory tract and by particle size.8 The percentages in figure 4 are based on the models by the International Committee on Radiologic Protection, averaged for males and females and activity levels. Most of the large particles (10 to 100 mcm) will be deposited in the upper (head) airways, while small particles (<1 mcm) are more likely to deposit in the alveolar (gas exchange) region of the lung.
Figure 4. Percentage of aerosol particles that are inhaled and deposit in the respiratory system, based on the International Committee for Radiologic Protection model.8

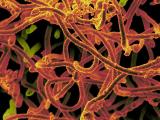
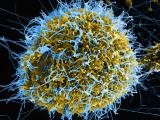
Ebola viruses have a diameter of 0.08 mcm, but they may be up to 14 mcm in length.9 Infectious microorganisms emitted in body fluid, however, are generally associated with proteins and other materials of the body fluid rather than "free." Thus, the infectious microorganism is present in particles with diameters that vary by several orders of magnitude. The deposition pattern of these particles in the respiratory tract may differ from the deposition of the "free" virus, but the key to developing infection is whether viruses are deposited on cells with receptors that will enable infection. Macrophages and dendritic cells infected by Ebola virus are found throughout the respiratory system. This means that a wide range of particle sizes carrying Ebola virus may deposit anywhere in the respiratory tract—from the nose or mouth to the alveoli—and initiate an infection.
By way of comparison, the bacterium Mycobacterium tuberculosis has a diameter of 0.2 to 0.5 mcm and a length of 2 to 4 mcm and initiates infection in the alveolar region of the lung. The influenza virus is much smaller and spherical—about 0.08 to 0.12 mcm in diameter—and initiates infection at sites from the nasal mucosa to the alveoli, depending on the preferred receptor of the virus strain.10 Both M tuberculosis and influenza viruses are emitted in cough particles with a wide variety of diameters and recognized as causing infection subsequent to inhalation near and at some distance from an infectious person.3,11
Ebola virus disease transmission
To understand how EVD is transmitted, it is helpful to consider both epidemiologic findings and the physical process by which the disease is transmitted.
Epidemiologic studies of past outbreaks suggest that three factors are linked to a high risk of person-to-person EVD transmission12-15:
- Caring for an infected person at home or in a healthcare setting
- Contact with the body fluids of an infected person—for example, while providing care
- Contact with an infected corpse
Considering these risk factors, we presume that infection can be transmitted to a susceptible person near an infected person.
To initiate infection, Ebola virus must be shed from an infectious person, and must enter cells in a susceptible person, where it can initiate infection. There is strong evidence that numerous bodily fluids contain Ebola virus. And there is good evidence that Ebola virus is capable of initiating infection in a variety of cell types that are widely distributed throughout the human body. Finally, several animal studies have provided evidence of aerosol transmission. Considering each component in turn:
- Ebola RNA has been found in the blood, breast milk, saliva, semen, stool, sweat, and urine of infected persons16-19 and has been detected from conjunctival, vaginal, rectal, and skin swabs.16,20 Viral inclusions have also been found within alveolar macrophages and viral particles detected within alveolar spaces.21 Viral RNA is typically more plentiful than culturable virus, so testing by quantitative polymerase chain reaction (qPCR) identifies an agent more frequently and in higher abundance than testing by culture does. The detection of viral RNA is assumed to indicate the presence of live virus capable of causing infection. While Ebola virus has been cultured from serum,22 saliva, breast milk, semen, and urine,16,18 tests of other body fluids have used only qPCR methods or had negative results by culture.
- Viral loads in serum increase during the course of illness, and a high viral load is associated with high fatality rates. Furthermore, body fluids may be copiously emitted in the late phases of disease.22,23 This emission pattern indicates that the risk of exposure to Ebola virus is highest when EVD patients are experiencing symptoms, particularly serious illness, and is consistent with epidemiologic analyses of risk factors and exposure histories.
- Cough can be a common symptom in EVD patients. A World Health Organization study last month on the first 9 months of the epidemic in West Africa found that 194 of 665 patients (29.6%) experienced coughing, and 2.4% (20 of 831) had a bloody cough.24 And in a smaller study last month of EVD patients in Sierra Leone, 16% had a cough (7 of 44), a rate that climbed to 21% in fatal cases (6 of 36).23
- Ebola virus can initiate infection only if it reaches cells in the susceptible person that present the appropriate receptors. Evidence indicates that Ebola virus may reach these cells through mucosal surfaces, breaks in the skin, or injection.9 A variety of cell types have the appropriate receptors, including monocytes, macrophages, dendritic cells, and others.9,25 Dendritic cells are found in tissues that have contact with the outside environment, such as skin, nose, lungs, stomach, and intestines. Macrophages are also located in those areas, as well as many other tissues throughout the body. Both cell types play an important role in fighting infections.
- In one study involving Ebola-inoculated rhesus macaques, two of the three control macaques died of EVD in spite of being housed about 3 meters from the inoculated macaques.26 In another study, two rhesus macaques receiving a low inhaled Ebola dose and two receiving a high inhaled dose developed rapidly fatal disease.27 And six Ebola-infected piglets were kept at least 20 cm from four caged macaques yet all the monkeys became infected in a setting that the authors described as most conducive to aerosol transmission.28
This information allows us to describe the ways in which EVD can be transmitted from one person to another:
- 1. Direct contact with infected body fluids
- Body fluid containing Ebola virus that comes in direct contact with the skin may enter the body through a break in the skin.
- Body fluid containing Ebola virus may transmit an infection if sprayed directly onto mucous membranes of the mouth, nose, or eyes.
- 2. Indirect contact with infected body fluids
- Body fluid containing Ebola virus can be present on an object and then transferred by the hands to the mouth, nose, or eyes.
- Medical equipment (eg, syringes) contaminated with a body fluid containing Ebola virus can break the skin and introduce the virus into the blood or other tissues.
- 3. Inhalation of infectious aerosols near an infected person
- The emission of body fluids containing Ebola virus—through vomiting, diarrhea, coughing, or hemorrhage—may generate aerosols containing virus that can be inhaled and deposited throughout the respiratory system.
- Medical procedures like intubation, bronchoscopy, drug delivery, assisted breathing, etc, may generate aerosols containing Ebola virus, which can be inhaled and deposited throughout the respiratory system.
Aerosol transmission recognizes that the spraying of body fluids containing Ebola virus directly onto mucous membranes is unlikely to occur in the absence of inhalation of infectious aerosols. Available data do not indicate that aerosol transmission at a distance from an infected person is an important route of Ebola virus transmission. In this we agree with statements from the CDC that the "airborne" (old paradigm) route of transmission (inhalation of infectious particles at a distance from the source) has not been documented in previous EVD outbreaks.
There are at least two explanations for why Ebola virus transmission has not been shown to occur at a distance from the source, even though data suggest that Ebola virus can remain viable in the air for some time (up to 90 minutes at room temperature and humidity).29 One explanation is that Ebola virus is not viable by the time it gets to point C (ie, inhalation of non-viable virus will not produce an infection). A second possibility is that the infectivity of Ebola virus upon inhalation of small particles is very low, so the probability of infection is too small to observe.
How to identify and manage the risk?
Healthcare workers caring for symptomatic patients with EVD have the greatest risk of exposure and infection through all the routes of transmission, as described above. Patients with severe symptoms will emit more bodily fluids—blood, vomitus, feces—than asymptomatic patients with EVD, and the emission of these fluids potentiates aerosol generation. Some medical procedures, such as intubation, bronchoscopy, and respiratory therapies, may generate aerosols and have also been shown to increase the transmission of acute respiratory infections.30
Other workers who may come into contact with people who have EVD include emergency responders, cleaners, transportation workers, and service workers. Of these, emergency responders may have the greatest chance of encountering a person with symptomatic EVD, since they may be called to aid or transport a symptomatic person. In general, all workers should avoid close contact with a person who has symptomatic EVD and his or her bodily fluids in the absence of PPE or other controls.
The selection of PPE and other controls should be informed by risk assessment. Every organization should conduct a risk assessment to determine who is at greatest risk and the level of protection they need to prevent infection. A risk assessment may be qualitative or quantitative, but it should consider factors that influence both the magnitude and probability of exposure. The magnitude of exposure is the number of Ebola viruses the worker may contact or inhale, given the presence of an infectious EVD patient. The probability of exposure describes the likelihood that the worker will encounter an infectious EVD patient.
A few examples are provided to illustrate the differences in risk for different work settings. These PPE recommendations should not be regarded as prescriptive but rather illustrative of the connection between risk levels and protection levels. PPE is only one method of preventing exposure. Other methods, such as engineering and administrative controls, should be employed first and may preclude the necessity for PPE altogether or lower the protection level needed. As well, working conditions, work settings, and the interaction of one type of PPE with another should be considered when selecting PPE.
- Healthcare workers caring for infected patients with advanced EVD symptoms have the highest risk of exposure by all routes of transmission and should be provided with complete body and respiratory protection. Their respirator should ensure they are protected when high concentrations of aerosolized body fluids are present.
- Negative pressure half-facepiece respirators, such as N95 filtering facepiece respirators and half-mask elastomeric respirators, offer the minimum level of protection of all respirator classes and may not offer adequate protection from aerosol transmission when patients are emitting copious amounts of body fluids. More appropriate respirators for such exposures are those with higher levels of protection, such as full-facepiece elastomeric respirators or positive pressure respirators with a hood or helmet.
- Emergency responders should have a high level of skin and respiratory protection available, and wear the PPE when a patient reports recent travel to an area with endemic EVD or recent contact with someone who had a travel history to the area or is known to have EVD, and has signs and symptoms compatible with EVD. Though the probability of encountering an EVD patient on any particular day may be small, high exposures are possible when an EVD patient is encountered because the patient may be symptomatic or require aerosol-generating medical procedures prior to or during transport. Healthcare workers in this setting should have a respirator that offers a high level of protection.
A half-mask negative pressure respirator may not offer adequate protection if aerosols are occurring from natural processes or medical procedures. A powered air-purifying respirator (PAPR) may be cumbersome and difficult to don quickly. A full-facepiece elastomeric respirator might be a better choice in this setting.
- Healthcare workers performing triage or working in an emergency department or in jobs with a similar probability of exposure should have PPE available to them that prevents direct contact with body fluids and inhalation of infectious aerosols. It may be possible to isolate healthcare workers or patients during triage, thus eliminating the need for PPE. Isolating potentially infected patients immediately following triage would also limit exposures. Those healthcare workers in direct contact with a suspected Ebola patient would require high levels of protection.
- A half-mask negative pressure respirator may not offer adequate protection if aerosols are occurring naturally or from medical procedures. A PAPR would be a much better choice for this setting.
- Workers in other sectors should have PPE available that is commensurate with their risk and job responsibilities. If they must interact directly with an infected person or his or her body fluids, they should be provided with full skin and respiratory protection. If they will only briefly interact with an infected person or the person's body fluids, they may require lower levels of PPE.
Currently the CDC recommends (here and here) that healthcare workers and emergency medical services personnel who provide care to people who may have EVD to cover all of their skin and wear respiratory protection. While this is consistent with our recommendations, the CDC guidelines do not recognize that different respirators offer different degrees of protection. An N95 filtering facepiece respirator is the least protective type of respirator available and will reduce outside concentrations by only 1/10th, which may not be adequate for the high concentrations of infectious aerosols likely during vomiting, diarrhea, or medical procedures.
In our previous commentaries on Ebola and MERS, we described a control banding approach for selecting respirators for aerosol-transmissible diseases. We encourage the use of this or similar tools in the risk assessment process to protect employees from infectious aerosols. These tools will lead to better PPE selections than are described in the current CDC guidelines.
References
- CDC. Guidance on personal protective equipment to be used by healthcare workers during management of patients with Ebola virus disease in U.S. hospitals, including procedures for putting on (donning) and removing (doffing). Oct 20, 2014 [Full text]
- IOM. Research priorities to inform public health and medical practice for Ebola virus disease: workshop in brief. Nov 14, 2014 [Full text]
- Seigel JD, Rhinehart E, Jackson M, Chiarello L, and the Healthcare Infection Control Practices Advisory Committee (CDC). 2007 Guidelines for isolation precautions: preventing transmission of infectious agents in healthcare settings. 2007 [Full text]
- Chao CYH, Wan MP, Morawska L, et al. Characterization of expiration air jets and droplet size distributions immediately at the mouth opening. J Aerosol Sci 2009 Feb;40(2):122-33 [Full text]
- Nicas M, Nazaroff WW, Hubbard A. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. J Occup Environ Hyg 2005 Mar;2(3):143-54 [Abstract]
- Evans MR, Meldrum R, Lane W, et al. An outbreak of viral gastroenteritis following environmental contamination at a concert hall. Epidemiol Infect 2002 Oct;129:355-60 [Abstract].
- Marks PJ, Vipond IB, Regan FM, et al. A school outbreak of Norwalk-like virus: evidence for airborne transmission. Epidemiol Infect 2003 Aug;131:727-36 [Abstract]
- Hinds WC. Aerosol technology. New York, NY: John Wiley & Sons, 1999 [Listing]
- Feldmann H, Geisbert TW. Ebola haemorrhagic fever. Lancet 2011 Mar 5;377(9768):849-62 [Abstract]
- Shinya K, Ebina M, Yamada S, et al. Influenza virus receptors in the human airway. Nature 2006 Mar 26;440:435-6 [Abstract]
- Tellier R. Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface 2009 Dec 6;6(suppl 6):S783-90 [Abstract]
- Dowell SF, Mukunu R, Ksiazek TG, et al. Transmission of Ebola hemorrhagic fever: a study of risk factors in family members, Kikwit, Democratic Republic of Congo, 1995. J Infect Dis 1999 Feb;179(suppl 1):S87-91 [Full text]
- Francesconi P, Yoti Z, Declich S, et al. Ebola hemorrhagic fever transmission and risk factors of contacts, Uganda. Emerg Infect Dis 2003 Nov;9(11):1430-7 [Full text]
- Roddy P, Howard N, Van Kerkhove MD, et al. Clinical manifestations and case management of Ebola haemorrhagic fever caused by a newly identified virus strain, Budibugyo, Uganda, 2007-2008. PLoS One 2012 Dec 28;7(12):e52986 [Full text]
- Wamala JF, Lukwago L, Malimbo M, et al. Ebola hemorrhagic fever associated with novel virus strain, Uganda, 2007-2008. Emerg Infect Dis 2010 Jul;16(7):1087-92 [Full text]
- Bausch DG, Towner JS, Dowell SF, et al. Assessment of the risk of Ebola virus transmission from bodily fluids and fomites. J Infect Dis 2007 Nov 15;196(suppl 2):S142-7 [Full text]
- Formenty P, Leroy EM, Epelboin A, et al. Detection of Ebola virus in oral fluid specimens during outbreaks of Ebola virus hemorrhagic fever in the Republic of Congo. Clin Infect Dis 2006 Jun 5;42(11):1521-6 [Full text]
- Kreuels B, Wichmann D, Emmerich P, et al. A case of severe Ebola infection complicated by gram-negative septicemia. (Brief report) N Engl J Med 2014 (published online Oct 22) [Full text]
- Richards GA, Murphy S, Jobson R, et al. Unexpected Ebola virus in a tertiary setting: clinical and epidemiologic aspects. Crit Care Med 2000 Jan;28(1):240-4 [Abstract]
- Rodriguez LL, De Roo A, Guimard U, et al. Persistence and genetic stability of Ebola virus during the outbreak in Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis 1999 Feb;179(suppl 1):S170–6 [Full text]
- Martines RB, Ng DL, Greer PW, et al. Tissue and cellular tropism, pathology and pathogenesis of Ebola and Marburg viruses. J Pathol 2014 (published online Oct 9) [Abstract]
- Towner JS, Rollin PE, Bausch DG, et al. Rapid diagnosis of Ebola hemorrhagic fever by referse transcription-PCR in an outbreak setting and assessment of patient viral load as a predictor of outcome. J Virol 2004 Apr;78(8):4330 [Abstract]
- Schieffelin JS, Shaffer JG, Goba A, et al. Clinical illness and outcomes in patients with Ebola in Sierra Leone. N Engl J Med 2014 (published online Oct 29) [Full text]
- WHO Ebola Response Team. Ebola virus disease in West Africa—the first 9 months of the epidemic and forward projections. N Engl J Med 2014 Oct 16;371(16):1481-95 [Full text]
- Bray M, Geisbert TW. Ebola virus: the role of macrophages and dendritic cells in the pathogenesis of Ebola hemorrhagic fever. Int J Biochem Cell Biol 2005 Aug;37(8):1560-6 [Abstract]
- Jaax N, Jahrling P, Geisbert T, et al. Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory. Lancet 1995;346(8991):1669-71 [Abstract]
- Johnson E, Jaax N, White J, et al. Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus. Int J Exp Pathol 1995 Aug;76(4):227-36 [Abstract]
- Weingartl HM, Embury-Hyatt C, Nfon C, et al. Transmission of Ebola virus from pigs to non-human primates. Sci Rep 2012 Nov 15;2:811 [Full text]
- Piercy TJ, Smither SJ, Steward JA, et al. The survival of filoviruses in liquids, on solid substrates and in dynamic aerosol. J Appl Microbiol 2010 Nov;109(5):1531-9 [Full text]
- Tran K, Cimon K, Severn M, et al. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One 2012 Apr 26;7(4):e35797 [Full text]