Mar 19, 2008 – ATLANTA (CIDRAP News) – Serious microbial threats, including drug-resistant influenza and foodborne pathogens, remain stubbornly persistent even as unpredictable new threats are emerging, researchers said this week at the leading international conference on new and resurgent infectious diseases.
Many of the threats are emerging in parts of the world too poor to fund adequate surveillance and control measures. And industrialized countries' spending on intercepting those globalized infections is not keeping pace with the need.
"Many of the challenges that face us right now are not likely to get better; in some ways, they are likely to get worse," Dr. Julie L. Gerberding, director of the Centers for Disease Control and Prevention (CDC), said during the opening speeches of the International Conference on Emerging Infectious Diseases, which the CDC sponsors along with several scientific organizations. "These problems can only be solved by the investment necessary to tackle them."
Research presented at the conference ranged from information on the complexities of controlling and treating influenza and other respiratory diseases to insights into foodborne disease transmission. And as always at such a large conference—a biennial gathering of 2,000 scientists giving roughly 500 papers and posters—there were the scientific equivalent of early-warning alarms.
In influenza news, CDC and state health department researchers found that:
- Adamantane drugs, the older of the two classes of influenza antivirals, are becoming increasingly useless against seasonal flu. A global survey of isolates collected during the 2006-07 flu season found 72% of H3N2 strains were resistant to adamantanes; in Asia, 100 percent of H1N1 strains were resistant, though 94% of US H1N1 strains remained vulnerable to the drugs.
- Meanwhile, resistance to neuraminidase inhibitors, the second class of flu drug, is creeping up. Between 2004 and the current flu season, the proportion of isolates resistant to neuraminidase inhibitors rose from 1% to 5% among all flu strains. Resistance to oseltamivir (Tamiflu), the more widely used drug in the class, rose to 9% among H1N1 strains.
- And in further confirmation that the current seasonal flu vaccine did not work as planned, an analysis of military flu-like illness statistics by the Naval Health Research Center in San Diego found the effectiveness of the flu shot against H1N1 strains was 71%, lower than recent CDC estimates.
In a warning of the stealthy nature of novel flu strains, a team from the University of Florida, the CDC's flu branch, and a pet-rescue program called HemoPet/Pet Life-Line found that canine influenza has been circulating without detection far longer than supposed. The disease, which kills by hemorrhagic pneumonia, was first detected in dogs in Florida in 2004 and has since spread to 25 states and Washington, DC. But according to the rescue program's blood-donor records, the strain has actually been in Florida dogs since 1999, and it may have caused unsolved respiratory disease outbreaks at dog tracks that year and in 2003.
Among the reports on foodborne illnesses:
- The proportion of disease outbreaks linked to leafy greens is rising faster than the consumption of lettuce and spinach, signaling a true increase in the incidence of greens-related foodborne illness, according to CDC researchers.
- Strains of Salmonella isolated from cattle slaughtered at plants monitored by the US Department of Agriculture showed significant increases between 1997 and 2005 in resistance to cephalosporins, a class of drugs used in both veterinary and human medicine. Proportions of isolates resistant to the veterinary drug ceftriaxone increased from 1% to 2.1%; to ceftiofur, from 0% to 21.6%; and to cefoxitin, from 9.1% to 19.8%.
- And research done at the University of Pennsylvania found that 22% of raw chicken purchased at retail outlets in central Pennsylvania in 2006 and 2007 was contaminated with Salmonella; 53% of the Salmonella isolates were resistant to at least one drug, and 45% were resistant to five drugs or more.
Blood and organ transplants are emerging as a rare and unpredictable route for transmission of infections, according to research presented at the conference, which featured reports of tuberculosis transmitted via transplant and fatal Group C streptococcal infection transmitted by transfused pooled platelets.
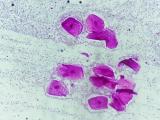
And in just two of many reports on the increasingly high-profile pathogen MRSA—methicillin-resistant Staphylococcus aureus, which causes both healthcare-acquired and community-acquired infections—CDC researchers reported a higher-than-predicted rate of community-acquired pneumonias due to MRSA. In addition, Dr. J. Scott Weese, a veterinarian from the Ontario Veterinary College, delivered preliminary results of a survey of 212 raw pork products purchased in four Canadian provinces that found a MRSA contamination rate of almost 10%.