Two new US studies explore mpox epidemiologic factors, with one showing that sexual activity remains an important route of exposure among patients not reporting male-to-male sexual contact (MMSC), and another finding that 1.3% of cases in the 2022-2023 global outbreak occurred in children and adolescents.
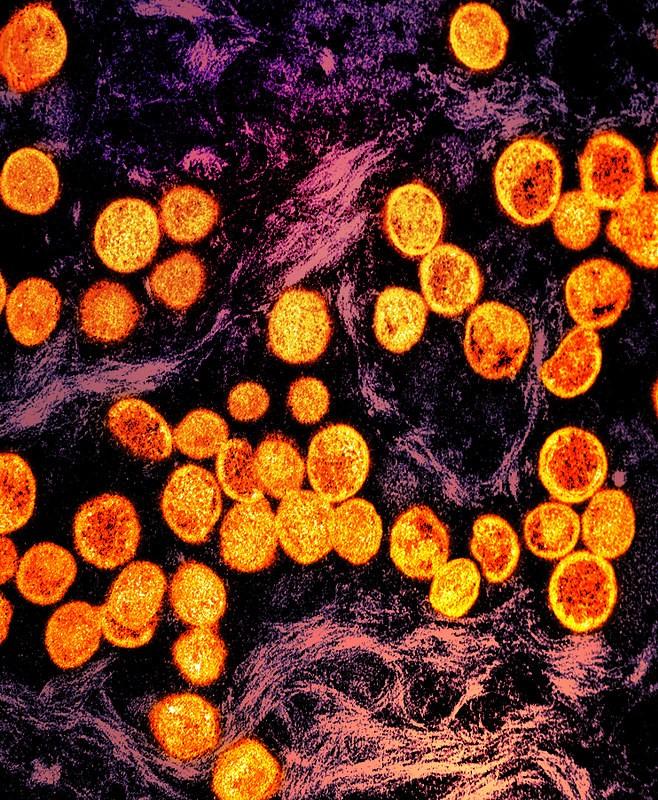
Mpox is a viral zoonotic disease that, until the outbreak began in May 2022, was primarily found in forested regions of Central and West Africa. During the outbreak, mpox was identified in many countries that previously had reported no cases, and by May 2023, more than 87,500 infections and 141 deaths were reported by 111 countries.
Household, sexual transmission
Today, Morbidity and Mortality Weekly Report published a study led by researchers from the US Centers for Disease Control and Prevention (CDC) on 122 mpox cases among the roughly 30% of patients who reported no MMSC in the 3 weeks before symptom onset or were missing exposure information in six jurisdictions from November to December 2022.
The jurisdictions included New York City and San Diego, California, and the states of California, Georgia, Louisiana, and Pennsylvania. The median patient age was 36 years, 50% were Black, 33% were Hispanic, and 10% were White.
A total of 62% of patients were cisgender men, 29% were cisgender women, and 6% were transgender women. Among the 45 patients who reported sexual orientation, 67% were heterosexual, 16% were gay or lesbian, and 13% were bisexual. Four of 32 patients (13%) didn't have secure housing or lived in a congregate setting.
Of 52 mpox patients who didn't report MMSC, 27% were exposed to someone with mpox through sexual activity (8 patients) or household contact (6). Among 38 patients without a known exposure to an infected person, 45% reported sexual activity, 37% cited close face-to-face contact, 29% attended large social gatherings, and 26% said they had spent time at work.
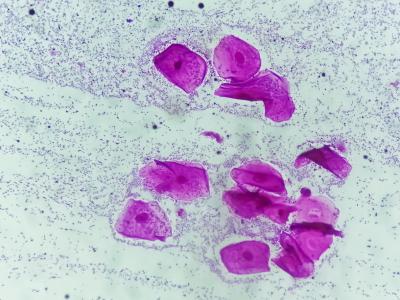
Nearly all of the 49 patients with symptom data (98%) reported having a rash, most commonly in the genital area (48%), followed by the legs (34%), arms (32%), and trunk (30%). Of the 32 patients reporting HIV status, 25% had HIV, and, of the 30 patients with mpox vaccination data, 10% had received at least one dose of the Jynneos mpox vaccine.
Highlighted case started with jail exposure
In the one identified household cluster, the index patient (patient A), a cisgender man, was exposed to mpox after spending 5 days in jail with as many as seven other people, including more than 10 hours with one who reportedly had characteristic mpox lesions on the arms. This person shared a water fountain, bench, and toilet with patient A, who began having symptoms the day after his release.
After returning home, patient A had sex with his female partner (patient B), whose symptoms started 1 week later. Patients A and B shared a home with a woman (patient C) and a preschooler, both of whom contracted mpox. Patient C's symptom onset occurred 2 weeks after patient B's, and the child’s symptoms started 1 week after patient C's.
Deploying Jynneos vaccine and focusing outreach and education to communities disproportionately affected by mpox should be prioritized to minimize health disparities.
"These findings suggest that sexual activity remains an important route of mpox exposure among patients who do not report MMSC," the researchers wrote. "Messaging for uninfected persons sharing or visiting a living space where a person with mpox resides should consider emphasizing maintenance of adequate hand hygiene; adhering to home cleaning and disinfection guidelines; and avoiding touching potentially contaminated surfaces or sharing personal items including bedding, clothing, towels, or utensils."
The authors recommended vaccination against mpox for people exposed to the virus or those at increased risk for infection. They also noted that the mpox patients in their study were disproportionately Black and Hispanic.
"Deploying Jynneos vaccine and focusing outreach and education to communities disproportionately affected by mpox should be prioritized to minimize health disparities," they wrote. "Coordinating with health departments, community-based organizations, and other partners can help achieve health equity in the current mpox outbreak."
Mpox in kids rare, mostly mild
A report published yesterday in Emerging Infectious Diseases shows that while the 2022-2023 multicountry mpox outbreak affected mainly men, 1.3% of the more than 87,500 cases occurred in children and adolescents, with one intensive care unit (ICU) admission and no deaths in that age-group.
World Health Organization (WHO) researchers analyzed global mpox surveillance data to determine the epidemiologic and clinical characteristics of the disease in patients younger than 18 years from January 2022 to May 2023.
The study authors noted that, from 1970 to 2021, 54% to 90% of mpox cases in Central Africa occurred in children, who experienced more severe illness and poor outcomes than adults.
Of the 1,118 pediatric cases in the study, most of them (61.8%) occurred in the Americas, followed by the Africa (30.3%), Europe (7.5%), Eastern Mediterranean, (<1%), and Western Pacific (<1%). No pediatric cases were reported in Southeast Asia.
The global proportion of pediatric mpox patients has consistently stayed at 0% to 3%. By May 2023, pediatric case counts were low in all regions, with the Americas, Eastern Mediterranean, and the Western Pacific reporting sporadic mpox infections in that age-group. Of the 1,102 children with mpox patients who had available data, 59.3% were boys and 40.7% were girls.
Of pediatric mpox patients with available hospitalization data, 47 of 335 (14.0%) were hospitalized, 1 required intensive care, and none died. Of the 166 patients with self-reported sexual orientation, 22.3% of those aged 13 to 17 years were men who have sex with men (MSM).
Eleven infected patients had HIV, one of whom had a weak immune system. Another six patients reported compromised immune systems caused by undisclosed medical conditions. A total of 67 of 293 (22.9%) infected patients with data had an epidemiologic link to a known mpox patient.
Clinicians should consider mpox as a possible diagnosis in these age groups when they have indicative symptoms, even with no known epidemiologic link to another case.
Patients aged 0 to 12 years contracted mpox mainly through physical, nonsexual person-to-person contact or contact with contaminated surfaces.
Of 542 patients with information, 87.1% had symptoms. Rash was the most common symptom among all age-groups (60%), and genital rash was reported by 54 of 229 (23.6%) of patients aged 13 to 17 years and by 19 of 313 (6.1%) of younger children. Among the 34 13- to 17-year-olds infected through sexual contact, 44.1% had a genital rash. Other common symptoms were fever (49.8%) and headache (29.2%). Lymphadenopathy was a feature of 11.1% of cases.
"The lower observed severity in children and adolescents in this outbreak than for previous outbreaks may be caused by a combination of increased ascertainment of mild cases, differing access to healthcare between settings, differing health status of the host populations, and lower virulence of clade IIb," which was implicated in 805 of 1,102 cases with clade information.
The researchers said the findings underscore the need for epidemiologic investigation of mpox in children and adolescents. "Clinicians should consider mpox as a possible diagnosis in these age groups when they have indicative symptoms, even with no known epidemiologic link to another case," they concluded.