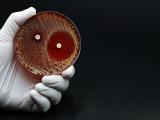
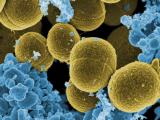
May 17, 2010 (CIDRAP News) A study designed to explore management of Staphylococcus aureus of hospitalized children found that methicillin-resistant (MRSA) infections rose tenfold over the 10-year study period, leading to dramatic changes in antibiotic prescribing patterns.
Although the rise in MRSA infections in hospitalized children wasn't surprising, the researchers said little was known about how the shift has affected overall treatment trends for S aureus illnesses.The findings, based on database information from 25 pediatric hospitals, appear today in an early online edition of Pediatrics.
The retrospective review looked at use of commonly prescribed antibiotics for S aureus from 1999 through 2008. Investigators measured the percentage of use for each drug and the length of therapy per 1,000 patient-days. Of 2.4 million discharges at the hospitals over the study time frame, 64,813 (3%) children were diagnosed with some form of S aureus infection. Skin and soft-tissue infections (SSTIs) were the most common type of infection, occurring more often in those with MRSA.
MRSA infections rose tenfold over the decade-long study period, but the rate for other S aureus infections held steady. By 2008 MRSA was responsible for 58% of all S aureus infections in hospitalized children, the group reported.
At the same time, the use of MRSA-targeted antibiotics for all S aureus patients rose from 52% to 79%, with clindamycin use rising threefoldmore than any other agents. Vancomycin use remained stable, while small increases were noted for trimethoprim-sulfamethoxazole (TMP/SMX) and linezolid..
Meanwhile, use of beta-lactam for S aureus infections decreased from 66% to less than 30%.
The group found similar patterns when they examined how long clinicians used the drugs, except for vancomycin, for which length of use increased.
When they singled out just patients with MRSA infections, the researchers also found similar patternsclindamycin use increased more than threefold, with smaller increases for TMP/SMX and linezolid. And again, though vancomycin use decreased, days of therapy with the drug increased for this group. Beta-lactam decreased in terms of both percentage and duration of use.
The authors also analyzed the data to see if infection site influenced antibiotic use. The largest increase in clindamycin use was for SSTIs and osteomyelitis. Though linezolid wasn't available during the first 2 years of the study, the researchers noted that its use increased substantially from 2001 though 2008. As with the other trends, beta-lactam use dropped significantly across the study period for all infection sites.
The group concluded that their findings suggest clinicians are becoming more comfortable with prescribing clindamycin for serious invasive S aureus infections. They wrote that trends suggest the drug may be replacing beta-lactams as front-line empiric therapy for patients who have presumed S aureus infections.
Given the dramatic increase in clindamycin use, clinicians should be aware of the drug's limitations, including resistance, which may vary geographically, and antibiotic pressure, which can lead to the development of resistance in clindamycin-sensitive MRSA strains, they wrote. "Therefore, it is essential that clinicians be aware of and continue to monitor their institution's antibiograms," they cautioned.
Prospective studies that compare empiric and definitive treatment for MRSA infections in children are needed to define the most appropriate approach, they added.
Herigon JC, Hersh AL, Gerber JS, et al. Antibiotic management of Staphylococcus aureus infections in US children's hospitals, 1999-2009. Pediatrics 2010 May 17;early online edition [Abstract]