- Pakistan reported two wild poliovirus type 1 (WPV1) cases this week, marking its first of 2024. Both patients experienced paralysis onset in February and are from Balochistan province, which has been one of the country's hot spots, the Global Polio Eradication Initiative (GPEI) said in its latest weekly update. Also, the country reported 21 more environmental detections of the virus, including 5 in Balochistan, 11 in Sindh, 3 in Khyber Pakhtunkhwa, and 1 each in Islamabad and Punjab. Elsewhere, four countries reported more cases involving circulating vaccine-derived poliovirus type 2: Guinea, Mali, Somalia, and Yemen.
- Three countries in the Americas have reported a total of seven yellow fever cases this year, according to an update yesterday from the Pan American Health Organization (PAHO). Of the seven cases, four were fatal. Countries reporting cases include Colombia, which confirmed three cases, all fatal, in people from different cities in Putumayo department in the south. Guyana reported two cases in people who worked at the same logging camp near the border with Brazil. Peru noted two confirmed case-patients in different departments. Both had been exposed to wooded or wild areas in their agricultural work. In a related development, Brazil reported detections in nonhuman primates. For comparison, four countries reported 41 cases in 2023. PAHO said the risk in the Americas remains high, because impacts from the COVID-19 pandemic have led to gaps in vaccine coverage.
- Blue Lake Biotechnology, a US-based vaccine company, yesterday announced promising preliminary findings from a phase 1/2a clinical trial of its intranasal vaccine against respiratory syncytial virus (RSV) in young children. In a press release, the company said the vaccine, called BLB201, is immunogenic and well tolerated, with no significant safety signals after a single intranasal dose. The trial is under way in seropositive children ages 18 to 59 months old. The company is currently enrolling seronegative and seropositive kids as young as 8 months old in the ongoing trial. The US Food and Drug Administration (FDA) has granted the company fast-track designation for the vaccine. The vaccine encodes the RSV F protein and uses a proprietary parainfluenza virus 5 vector, not known to cause human disease.
Quick takes: Polio in Pakistan, yellow fever in the Americas, intranasal RSV vaccine trial
US flu activity declines, along with other respiratory viruses
Flu activity finally declined last week following a lengthy post-holiday bump, though levels are still elevated, the Centers for Disease Control and Prevention (CDC) said today in its latest weekly FluView report.
In its weekly respiratory virus snapshot, the CDC said indicators of COVID and respiratory syncytial virus (RSV) also declined. For all three viruses, test positivity and emergency department visits declined last week. Nine jurisdictions reported high or very high activity, down from 17 the previous week.
Flu up slightly in Pacific Northwest
For flu, activity decreased or was stable in nine regions but increased slightly in the Pacific Northwest. Of respiratory samples that were positive for flu at public health labs, 64.6% were influenza A, and of subtyped influenza A viruses, 56.1% were H3N2, and 43.9% were 2009 H1N1.
Hospitalizations have been declining since January, and overall deaths also trended downward. However, the CDC reported five more pediatric flu deaths, raising the total to 121 for the season. Two were due to H1N1, and three involved influenza B.
COVID wastewater detections decline to low level
In its latest COVID data updates, most indicators show a continuing steady decline, though deaths were level.
Wastewater detections of SARS-CoV-2 are now classified as low. Levels are still highest in the south, but they have declined steeply in recent weeks.
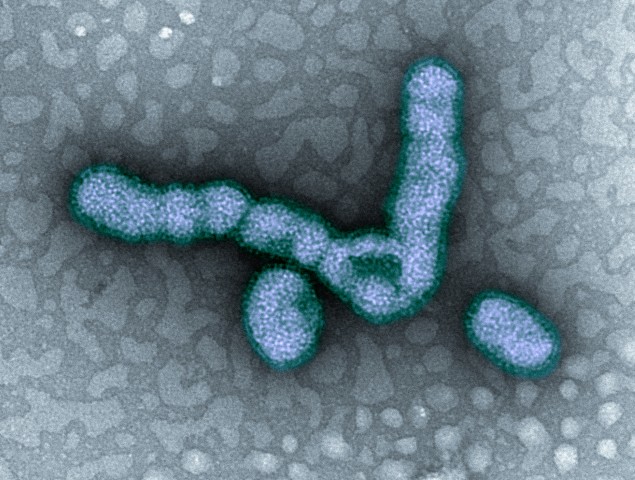
Vietnam probes human H5 avian flu case
Health officials in Vietnam's Khanh Hoa province have confirmed an H5 avian flu infection in a 21-year-old university student, though there are no details yet on the strain or how the patient contracted the virus.

Details about the case were reported in Vietnamese media reports translated and posted by Avian Flu Diary, an infectious disease news blog. An official statement on the case from provincial health officials was translated and posted by FluTrackers, an inflection disease news message board. Khanh Hoa is on Vietnam's southeastern coast.
Man hospitalized in serious condition
The patient's symptoms began on March 11, and he returned home a few days later, where he stayed with his mother and sister while seeking medical care. When his symptoms worsened, he was hospitalized at a regional hospital. Soon after, he was transferred to Khanh Hoa provincial hospital where healthcare workers collected samples and sent them to the Pasteur Institute in Nha Trang, which revealed the H5 influenza virus.
The man is hospitalized in serious condition and in isolation at the Provincial Hospital of Tropical Diseases. Health officials are monitoring contacts, including family members, health workers, and university students.
So far, the subtype isn't known, but a few human cases involving older and recent H5N1 virus clades have been reported over the past few years, and China and Laos have reported H5N6 infections.
The reports didn't say how the patient likely contracted the virus.
Study finds bivalent COVID vaccine not tied to stroke risk
Earlier this week in JAMA, researchers published data on the risk of stroke among Medicare beneficiaries aged 65 years and older in the immediate weeks following a bivalent (two-strain) COVID-19 vaccine dose, finding no significantly elevated risk during the first 6 weeks following injection.
The study comes a year after reports appeared in the US Vaccine Safety Datalink showing that during the immediate period (1 to 21 days) after vaccination, older adults were suffering more strokes if they received both the Pfizer bivalent COVID vaccine and a high-dose or adjuvanted influenza vaccine on the same day.
The authors used Medicare recipient data to estimate the risk among those who received either the Pfizer or Moderna COVID-19 bivalent vaccine, concomitant (same-day) administration of either brand of COVID vaccine plus a high-dose or adjuvanted flu vaccine, and a high-dose or adjuvanted flu vaccine within the first 1 to 21-day or 22-to-42-day risk window compared with the 43-to-90-day control window. Adjuvanted vaccines include a substance that boosts immune response.
Possible stroke risk with high-dose flu vaccine
The study included 5,397,278 Medicare beneficiaries who received either brand of the COVID-19 bivalent vaccine (median age 74 years; 56% were women), 11,001 of whom had a stroke during the study period.
The authors found no significant association for stroke with either COVID vaccine, but same-day administration of either brand and a high-dose or adjuvanted influenza vaccine was associated with an elevated risk of stroke.
The observed association between vaccination and stroke in the concomitant subgroup was likely driven by a high-dose or adjuvanted influenza vaccination.
"The current study additionally found an association that was small in magnitude between stroke and administration of a high-dose or adjuvanted influenza vaccine when the vaccine was administered without concomitant administration of either brand of the COVID-19 bivalent vaccine," the authors concluded. "This finding suggests that the observed association between vaccination and stroke in the concomitant subgroup was likely driven by a high-dose or adjuvanted influenza vaccination.”
Scientists caution about CDC guidance on over-the-counter drugs for COVID-19

In its most recent guidelines on the use of over-the-counter (OTC) drugs for COVID-19, the US Centers for Disease Control and Prevention (CDC) says that mildly ill patients can relieve symptoms such as fever and sore throat with acetaminophen or ibuprofen, but a team led by Florida Atlantic University (FAU) researchers says it's not that simple..
In a review in the American Journal of Medicine, the investigators conclude that the decision to take acetaminophen (eg, Tylenol), aspirin, or ibuprofen (eg, Motrin, Advil) should be done on an individual basis under the guidance of a clinician.
This is because the drugs aren't risk-free, with overuse of acetaminophen tied to irreversible liver damage, liver failure, the need for liver transplant, and kidney damage, the authors noted.
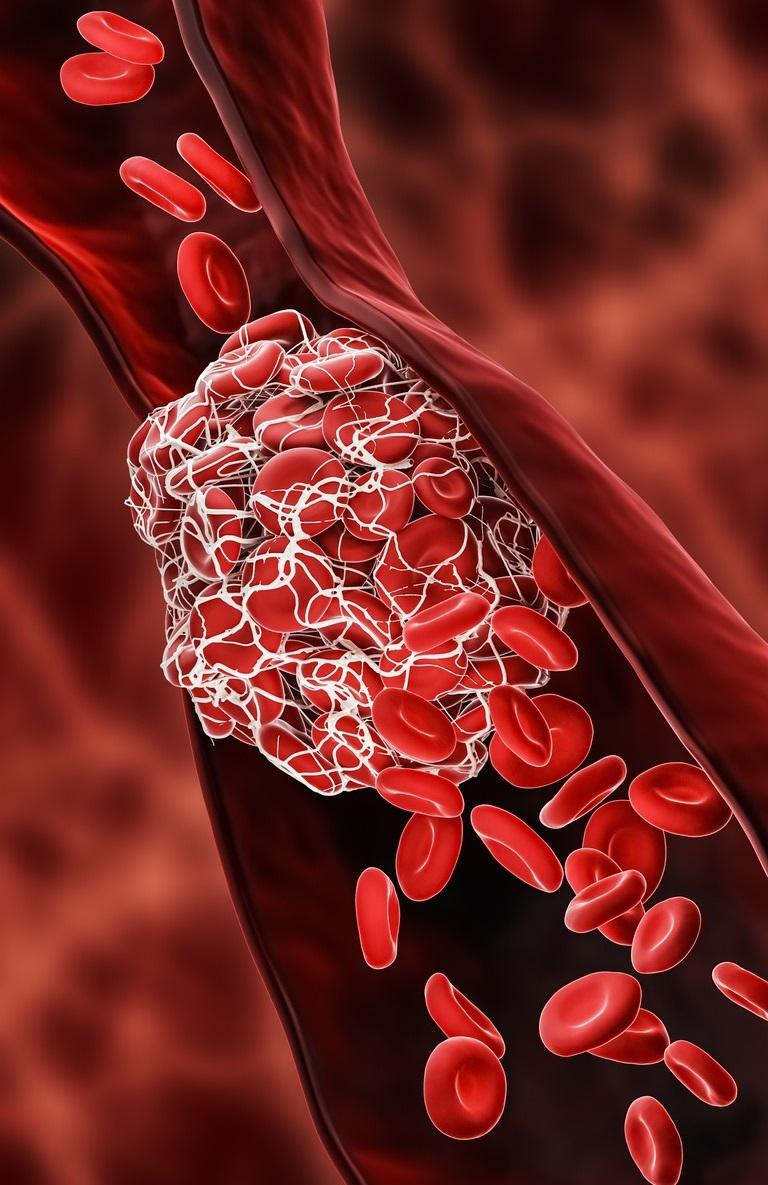
While aspirin's anti-inflammatory properties may be useful in treating moderate to severe COVID-19, it carries the risk of bleeding, especially in the gastrointestinal (GI) tract. This is of particular concern in COVID-19, which may itself lead to bleeding and clotting abnormalities.
Patient profile should guide decision, authors say
Compared with aspirin, ibuprofen, naproxen (eg, Aleve), and other non-steroidal anti-inflammatory drugs (NSAIDs) have greater adverse-event profiles, namely for gastroenteritis (inflammation of the GI tract) and peptic ulcers. As with acetaminophen, long-term use of these drugs can lead to liver and kidney toxicity.
We believe that health care providers should make individual clinical judgments for each of his or her patients in the selection of OTC drugs to treat symptoms of COVID-19.
Charles Hennekens, MD, DrPH
"Further, NSAIDs do not confer the cardiovascular benefits of aspirin," the authors wrote. "Since NSAIDs may induce a procoagulant state, the risks of thrombotic and thromboembolic events that can occur with a COVID-19 infection suggests that aspirin may have more beneficial effects in patients with acute COVID-19 infection."
They added that national guidelines should be based on evidence from large randomized trials and directed only to clinicians.
"We believe that health care providers should make individual clinical judgments for each of his or her patients in the selection of OTC drugs to treat symptoms of COVID-19," senior author Charles Hennekens, MD, DrPH, of FAU, said in a university news release. "This judgement should be based on the entire benefit to risk profile of the patient."
In case you missed it
This week's top reads
Our underwriters
Unrestricted financial support provided by











