A new Fair Health study shows that sexually transmitted disease (STD) diagnoses in the United States climbed 4.8% from 2020 to 2023, with a 23.8% surge in people aged 65 and older.
Fair Health researchers analyzed data from the nonprofit's repository of more than 47 billion commercial health insurance claims over the 3-year period. The results, released as an infographic, also describe a rise of 16.2% among Americans aged 55 to 64, 8.6% among 35- to 44-year-olds, 7.6% for those aged 45 to 54, and decreases of 6.6% for 19- to 24-year-olds and 3.8% for the 18-and-younger group.
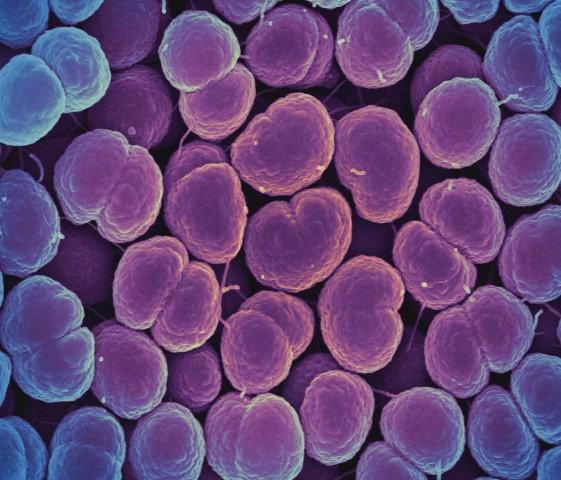
Syphilis, gonorrhea, HIV, and HPV
The fastest-growing STD diagnoses were syphilis (29.4%), gonorrhea (16.8%), and HIV/AIDS (14.1%). Among people aged 65 and older and 55 to 64, the largest increases (32.2% and 21.9%, respectively) were for human papillomavirus (HPV). Diagnoses of HPV also rose for those 45 to 54 (11.3%) and 35 to 44 (3.6%) but declined for those aged 19 to 24 (18.2%) and 25 to 34 (0.9%).
Syphilis diagnoses rose among both sexes (22.9% among males and 46.5% among females).
Diagnoses of gonorrhea grew 59.2% among male patients and fell 19.3% among females. Syphilis diagnoses rose among both sexes (22.9% among males and 46.5% among females).
"It is central to Fair Health’s mission to use our vast repository of claims data to provide data on public health concerns and support research by others," Robin Gelburd, JD, Fair Health president, said in a news release from the New York-based organization. "We hope this information brings greater clarity to the incidence of STDs."













