A trio of papers published this week in The Lancet Infectious Diseases make the case that meningitis vaccines could play a role in preventing gonorrhea infections.
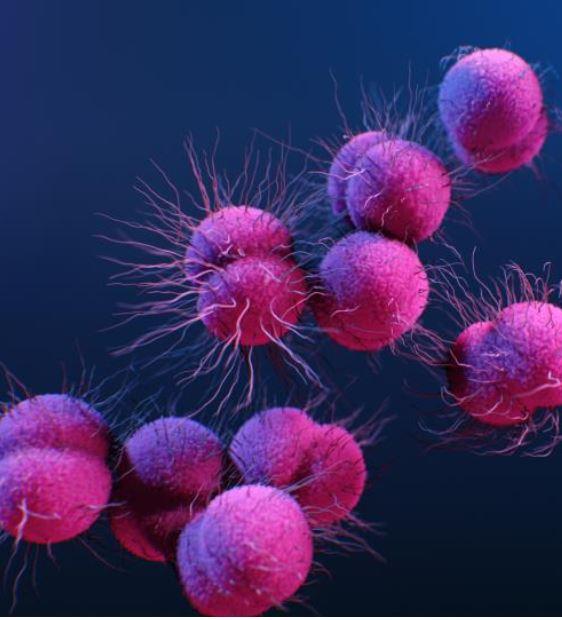
Gonorrhea is one of the most common sexually transmitted infections (STIs), with more than 82 million new infections recorded worldwide in 2020 and global incidence rising. And with resistance to the last remaining antibiotics recommended for gonorrhea treatment also on the rise, there are growing concerns that treatment options are becoming increasingly limited. That's led the World Health Organization (WHO) to label Neisseria gonorrhoeae a priority pathogen.
Given the concerns about how quickly gonorrhea develops resistance to antibiotics, vaccines have been suggested as a possible solution. While no gonorrhea-specific vaccines are currently available, two of the studies published in The Lancet found that the four-component serogroup B meningococcal (4CMenB) vaccine, designed against Neisseria meningitidis, showed some cross-protection against N gonorrhoeae.
And a third study suggests that the use of the 4CMenB vaccine in those at greatest risk of infection could be the most impactful and cost-effective method of averting gonorrhea.
Evidence of cross-protection
In an observational surveillance study, researchers from the Centers for Disease Control and Prevention (CDC), the Philadelphia Department of Health, and the New York City Department of Health and Mental Hygiene identified laboratory confirmed cases of gonorrhea and another STI, chlamydia, among 16- to 23-year-olds in Philadelphia and New York City from 2016 to 2018.
They then linked those cases to immunization registry records to determine how many of those individuals had received the 4CMenB vaccine, which has been recommended for that age-group for short-term protection against serogroup B meningococcal disease.
The researchers identified 167,706 infections (18,099 gonorrhea, 124,876 chlamydia, and 24,731 co-infections) among 109,737 individuals linked to the immunization registries. Of those individuals, 4,032 had received one dose of the 4CMenB vaccine (partial vaccination), 3,596 had received two doses (complete vaccination), and 64 had received three doses.
After adjusting for race, ethnicity, gender, and jurisdiction, they found that, compared with no vaccination, the complete vaccination series was 40% effective against gonorrhea (adjusted prevalence rate [aPR], 0.60; 95% confidence interval [CI], 0.47 to 0.77), and partial vaccination was 26% effective against gonorrhea (aPR, 0.74; 95% CI, 0.63 to 0.88). The vaccine was not effective against gonorrhea and chlamydia co-infection.
"These findings suggest that MenB-4C could offer cross-protection against N gonorrhoeae and provide further evidence supporting feasibility of an effective gonococcal vaccine," the study authors wrote. "A vaccine, even of modest effectiveness (30–50%) and duration of protection (2–4 years), might have a substantial effect on gonorrhoea prevention."
In another observational study, conducted in Australia, a team led by researchers from the University of Adelaide evaluated the impact and effectiveness of South Australia's 4CMenB vaccination program—which covers children ages 0 to 3, adolescents ages 15 to 16, and teens and young adults ages 17 to 20—against both meningitis and gonorrhea.
Two years after introduction of the vaccination program in 2019, among the nearly 100,000 adolescents and young adults who had received the 4CMenB vaccine, the researchers found that two doses of vaccine were 32.7% (95% CI, 8.3% to 50.6%) effective against gonorrhea infection, based on a case-control analysis using age-matched individuals with chlamydia infections as controls.
"Our study showed a reduction in serogroup B meningococcal disease cases among vaccine-eligible infants, high vaccine effectiveness against serogroup B meningococcal disease in vaccine-eligible cohorts, and cross-protection against gonorrhoea in adolescents and young adults," the study authors wrote.
Potential for averting cases, saving money
The third paper is a modeling study, in which researchers from Imperial College London, the University of Warwick, and Public Health England set out to estimate the impact and cost-effectiveness of using the 4CMenB as a gonorrhea vaccine. They focused on men who have sex with men (MSM), a group that has the highest per-capita rate of gonorrhea in England.
Using an integrated transmission-dynamic health model, the researchers compared four approaches for vaccinating MSM: vaccinating adolescents in schools before they become sexually active (vaccination before entry, VbE); vaccinating all MSM attending sexual health clinics (vaccination on attendance, VoA); vaccination on gonorrhea diagnosis (VoD); and vaccination according to risk of infection (VaR), with risk being indicated by current gonorrhea infection or more than 5 sexual partners per year.
Vaccine impact and cost-effectiveness was assessed relative to no vaccination.
The analysis found that VoA and VaR would have the largest impact, but the VaR strategy would be much more cost-effective because it would use fewer doses of vaccine. The model estimated that administering the 4CMenB vaccine under the VaR strategy, with a vaccine that is around 31% protective, would avert 110,200 gonorrhea cases, add 100.3 quality-adjusted life years (QALYs), and save £7.9 million (US $10.3 million) over 10 years.
"With a gonorrhoea-specific vaccine likely to take years to develop, a key question for policymakers is whether the meningitis vaccine 4CMenB should be used against gonorrhoea infection," senior author Peter White, PhD, of Imperial College London, said in a Lancet press release. "Our analysis suggests that giving the vaccine to those at the greatest risk of infection is the most cost-effective way to avert large numbers of cases."
White and his colleagues note that their analysis was conservative because of uncertainty about the level of protection 4CMenB offers against gonorrhea, and that they did not take into account the expected future burden of antibiotic-resistant gonorrhea. They also say that future development of gonorrhea-specific vaccines should prioritize increasing efficacy over duration of protection.
In an accompanying commentary, experts from the China-Australia Joint Research Center for Infectious Diseases who were not involved in the modeling study say that, given the rising global incidence of gonorrhea, the threat of multidrug resistance, and the WHO's target of 90% reduction in incidence by 2030, the findings suggest that policymakers should consider the 4CMenB vaccine as a potential option for gonorrhea prevention and control.
"The key message of the study is that vaccination using the 4CMenB vaccine according to the risk of the targeted MSM population is likely to be cost-effective, even if the vaccine were to have a relatively low efficacy and a short duration of protection," they wrote. "Such a strategy should be recommended and rolled out in a high-income country setting such as England.