A systematic review and meta-analysis found high rates of resistance to older and newer antibiotics in strains of hypervirulent Klebsiella pneumoniae (hvKp), researchers reported last week in the Journal of Global Antimicrobial Resistance.
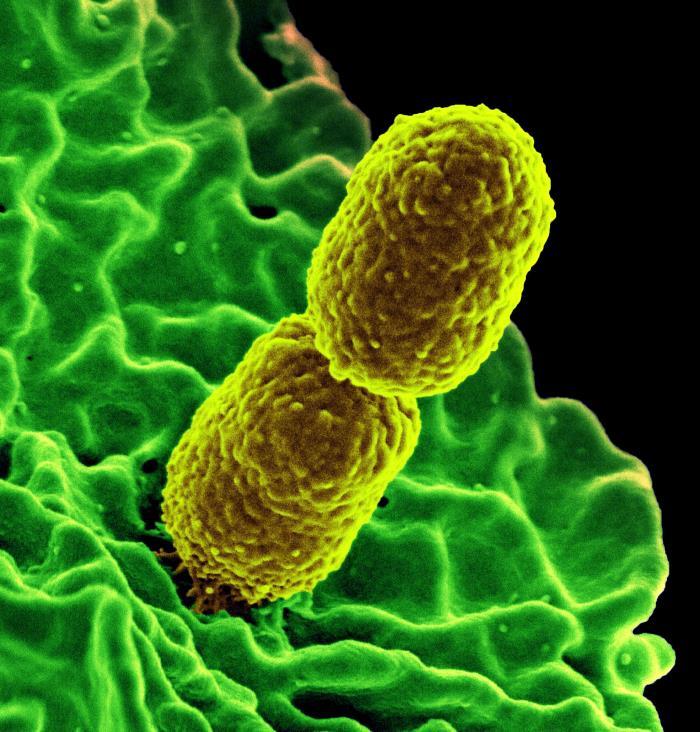
Although K pneumoniae has long been recognized as an opportunistic pathogen that can cause a wide range of infections in vulnerable, immunocompromised hospital patients, hvKp strains have emerged in recent years as a new threat. In contrast to "classic" K pneumoniae strains, hvKp can cause severe infections in healthy individuals that quickly disseminate to various body sites. And while initial hvKp strains were limited to Asia and were rarely resistant to antibiotics, they've spread globally and acquired multiple antibiotic resistance genes.
"The convergence of hypervirulence and antibiotic resistance in these strains presents a formidable challenge as traditional treatment options have become increasingly limited," researchers from the Pasteur Institute of Iran wrote.
A 'burgeoning public health challenge'
In their meta-analysis of 77 studies from 17 countries across 4 continents, the researchers found high rates of resistance in hvKp to older antibiotics, including ampicillin (95%), ampicillin/sulbactam (45.1%); third-generation cephalosporins, including cefotaxime (64.2%) and ceftazidime (55.9%); and the carbapenem antibiotics imipenem (44.8%), meropenem (51.4%), and ertapenem (42.6%). Quinolones, such as ciprofloxacin and levofloxacin, exhibited resistance of 46.3% and 35.5%, respectively, while azithromycin resistance was prevalent at 76.3%. Among newer antibiotics, colistin, fosfomycin, and nitrofurantoin resistance rates were 15.3%, 51.1%, and 39.2%, respectively.
The convergence of hypervirulence and antibiotic resistance in these strains presents a formidable challenge as traditional treatment options have become increasingly limited.
The meta-analysis also found a trend of increasing resistance to several antibiotics over time, significant differences in resistance across countries and regions, and variabilities in testing methods and standards.
The authors say global collaboration, standardized testing protocols, and tailored regional interventions will be needed effectively combat the threat of resistance in hvKp strains.
"This study serves as an urgent call for healthcare professionals, researchers, and policymakers to address this burgeoning public health challenge, and significantly contributes to the understanding of antibiotic resistance in hvKp strains, offering valuable insights for future research, clinical practice, and the development of public health policies," they wrote.