- The Michigan Department of Agriculture and Rural Development (MDARD) today announced another avian influenza outbreaks at a dairy farm, its first since July 9, raising the state's total to 27. The outbreak also marks the first from Van Buren County, putting the number of affected Michigan counties at 11. MDARD said samples will be sent to the US Department of Agriculture (USDA) for confirmation. In other avian flu developments, an H5N1 outbreak has been detected in backyard poultry in Florida's Hendry County in the south central part of the state, according to the latest update from the USDA Animal and Plant Health Inspection Service (APHIS).
- The World Health Organization (WHO) today announced the launch of a new initiative to speed the development of and access to mRNA vaccines against H5N1 avian influenza for people in low- and middle-income countries. The project is led by Argentina-based Sinergium Biotech, which has developed candidate H5N1 vaccines, and leverages the WHO and Medicines Patent Pool mRNA technology transfer program. The company's next step is to develop a preclinical data package, which will then be shared with other manufacturing partners.
- The USDA Food Safety and Inspection Service (FSIS) today unveiled a proposed rule to reduce Salmonella contamination and illnesses in raw poultry, noting the plan is part of a 3-year effort to reevaluate the strategy for controlling Salmonella rate in poultry products. The proposal addresses Salmonella contamination at poultry slaughterhouses and processors. The proposal would establish product standards that would prevent raw chicken carcasses, chicken parts, ground chicken, and ground turkey from entering commerce if they contain any Salmonella above 10 colony-forming units and any detectable level for certain serotypes of public health significance. The proposal would also require establishments to develop microbial monitoring programs. Comments on the proposal are due 60 days after Federal Register publication.
Quick takes: More avian flu in Michigan cows, mRNA H5N1 vaccine initiative, reducing Salmonella in raw poultry
SARS-CoV-2 widespread in Virginia wildlife, likely from people

An examination of 23 common wildlife species in Virginia finds evidence of SARS-CoV-infection in 6 and antibodies indicating previous infection in 5.
For the study, published today in Nature Communications, Virginia Tech researchers collected 789 nasal and oral swabs and 126 blood samples from animals live-trapped and released or being treated at wildlife rehabilitation centers in Virginia and Washington, DC, from May 2022 to September 2023.
Most animal exposures near human interfaces
Deer mice, opossums, raccoons, groundhogs, Eastern cottontail rabbits, and Eastern red bats had signs of infection, and isolates from an opossum showed previously unreported viral mutations closely matching the SARS-CoV-2 Omicron variant circulating in people at the time, which the authors said suggests at least seven recent human-to-animal virus transmission events. The mutations could alter the virus's effects on people.
The team also identified two mice on the same day with the same variant, indicating that one mouse infected the other or that they both were infected by the same person.
Further supporting human-to-animal viral spread was the finding of the highest SARS-CoV-2 antibody seroprevalence near hiking trails and other public areas. Some opossums, raccoons, Eastern gray squirrels, white-footed mice, and deer mice had SARS-CoV-2 antibodies.
The virus is indifferent to whether its host walks on two legs or four.
Carla Finkielstein, PhD
Transmission could have taken place via wastewater, trash bins, or discarded food. There was no evidence of animal-to-human transmission.
"The virus can jump from humans to wildlife when we are in contact with them, like a hitchhiker switching rides to a new, more suitable host," co-senior author Carla Finkielstein, PhD, said in a Virginia Tech press release. "The virus aims to infect more humans, but vaccinations protect many humans. So, the virus turns to animals, adapting and mutating to thrive in the new hosts."
SARS-CoV-2 infections have been previously identified in wildlife such as white-tailed deer and mink. "The virus is indifferent to whether its host walks on two legs or four," Finkielstein said.
The study team called for more research into how SARS-CoV-2 spreads from people to wildlife, within species, and from one species to another.
Most antibiotic prescriptions for kids' ear infections are too long, study finds

A study conducted at two large pediatric academic healthcare systems found that three-quarters of antibiotic prescriptions for children with ear infections were longer than recommended, researchers reported last week in the Journal of the Pediatric Infectious Diseases Society.
Using electronic medical record (EMR) data, researchers analyzed outpatient encounters for acute otitis media (AOM) in children ages 2 to 17 years at 135 care locations affiliated with Vanderbilt University Medical Center (VUMC) and Washington University from 2019 through 2022. The primary outcome was the proportion of 5-day antibiotic prescriptions. The researchers also looked at the proportion of 7-day and 10-day prescriptions, as well as treatment failure, AOM recurrence, hospitalization, and adverse drug events.
AOM accounts for roughly 25% of all antibiotics prescribed to children annually. The American Academy of Pediatrics AOM guidelines, published in 2013, recommend durations of 5 to 7 days for children ages 2 years and older with uncomplicated AOM. But previous studies have found most children receive longer durations.
75% of prescriptions were for 10 days
Of the 73,198 AOM encounters included in the study, 61,612 (84%) resulted in an antibiotic prescription, and only 3,144 (5%) of those prescriptions were for 5 days; 12,060 (20%) were for 7 days and 45,689 (75%) were for 10 days. Ten-day durations were more common at Washington University than VUMC (78% vs 70%) while 7-day prescriptions were more common at VUMC (25% vs 17%). Non-first line antibiotics were prescribed in 30% of cases.
Across both health systems, treatment failure, AOM recurrence, hospitalization, and mastoiditis were rare, as were office, emergency department, or urgent care visits for AOM within 30 days of the index visit.
The study authors say interventions to promote more widespread use of shorter durations for AOM in pediatric outpatient settings are urgently needed.
"Antibiotic prescribing for AOM is an important opportunity to improve antibiotic stewardship in children," they wrote. "Shortening durations of therapy for AOM has the potential to markedly reduce antibiotic exposure among children; this may lead to important reductions in the development of antibiotic resistance, adverse events, and other unintended consequences of antibiotics."
More illnesses reported in multistate Listeria outbreak linked to deli meats
Six more people have been sickened in a Listeria monocytogenes outbreak linked to deli meat, with one more state reporting an illness, the Centers for Disease Control and Prevention (CDC) said in a July 26 update. The new cases push the total from the outbreak, first announced on July 19, to 34 cases from 13 states. Two earlier deaths were reported.
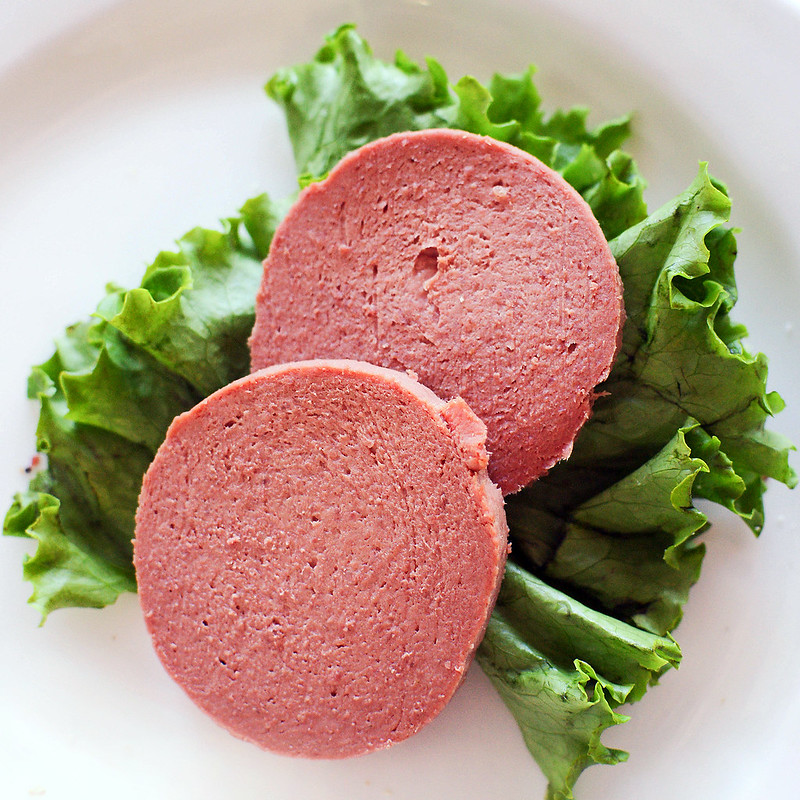
Since the outbreak was first announced, interviews with sick patients suggested some had eaten deli meat sliced or prepared at delis. Labs in Maryland have identified Listeria in an unopened package of Boar's Head liverwurst as part of the outbreak investigation, which prompted a recall of that and eight other deli meats that the company produced on the same line and the same day as the liverwurst.
The CDC said whole genome sequencing is underway to determine if the strain from the liverwurst sample is the same as the one making people sick. The US Department of Agriculture is conducting a traceback investigation to identify the suppliers of the deli meats bought by people sickened in the outbreak.
Health officials probe connection to other deli meats
The latest illness onset was July 12. Of information available on 33 patients, all were hospitalized. One patient got sick during pregnancy and remained pregnant after recovery. Pregnant women, seniors, and those with weakened immune systems are especially vulnerable to listeriosis complications
Though the products were distributed to retail delis nationwide, the states reporting cases are all in roughly the eastern half of the United States, with New York the hardest hit state with 12 cases, followed by Maryland with 6.
Of 24 people who were interviewed about their food exposures, 23 reported eating meats sliced at a deli. Of 23 who answered about liverwurst, 13 said they had eaten liverwurst before they became ill, and 7 reported the Boar's Head brand. "This information suggests that liverwurst is a likely source of this outbreak. CDC continues to gather information to understand which deli meats are causing illness in this outbreak," the group said.
CEPI announces clinical trial of post-exposure mpox vaccine
The Coalition for Epidemic Preparedness Innovations (CEPI) announced over the weekend a clinical trial set to launch in the Democratic Republic of Congo (DRC) and other African countries, which will assess whether the Bavarian Nordic mpox vaccine can protect people against the disease after they have come into contact with the virus.
The trial will also assess if vaccinated individuals who contract mpox have more mild courses of illness.
Trial to include DRC households
The DRC is currently experiencing a large mpox outbreak, with more than 11,000 cases and 443 deaths reported, many in children. The trial will be conducted in households in the DRC, Uganda, and Nigeria with a laboratory-confirmed mpox infection. CEPI will enroll more than 1,500 participants over the age of 10 years.
Participants will receive either an mpox vaccine or a placebo, and infections will be assessed 4 weeks later. Severity of infections, including number of lesions, will also be monitored.
While healthcare workers typically vaccinate somebody before they are at risk of an infection, post-exposure-vaccinations allow for a more targeted approach, minimizing use of vaccine supply.
"While healthcare workers typically vaccinate somebody before they are at risk of an infection, post-exposure-vaccinations allow for a more targeted approach, minimizing use of vaccine supply. Here, individuals in high-risk groups—such as household contacts of an index case—are vaccinated to potentially reduce the risk of infection, improve survival odds and stop onward chains of transmission," said CEPI CEO Richard Hatchett, MD, in a press release.
Review and meta-analysis finds high rates of antibiotic resistance in hypervirulent Klebsiella
A systematic review and meta-analysis found high rates of resistance to older and newer antibiotics in strains of hypervirulent Klebsiella pneumoniae (hvKp), researchers reported last week in the Journal of Global Antimicrobial Resistance.
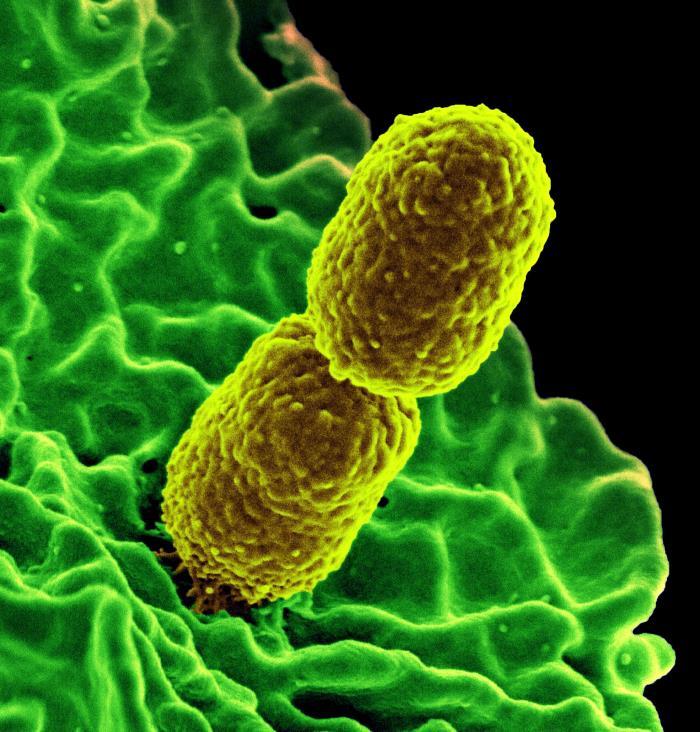
Although K pneumoniae has long been recognized as an opportunistic pathogen that can cause a wide range of infections in vulnerable, immunocompromised hospital patients, hvKp strains have emerged in recent years as a new threat. In contrast to "classic" K pneumoniae strains, hvKp can cause severe infections in healthy individuals that quickly disseminate to various body sites. And while initial hvKp strains were limited to Asia and were rarely resistant to antibiotics, they've spread globally and acquired multiple antibiotic resistance genes.
"The convergence of hypervirulence and antibiotic resistance in these strains presents a formidable challenge as traditional treatment options have become increasingly limited," researchers from the Pasteur Institute of Iran wrote.
A 'burgeoning public health challenge'
In their meta-analysis of 77 studies from 17 countries across 4 continents, the researchers found high rates of resistance in hvKp to older antibiotics, including ampicillin (95%), ampicillin/sulbactam (45.1%); third-generation cephalosporins, including cefotaxime (64.2%) and ceftazidime (55.9%); and the carbapenem antibiotics imipenem (44.8%), meropenem (51.4%), and ertapenem (42.6%). Quinolones, such as ciprofloxacin and levofloxacin, exhibited resistance of 46.3% and 35.5%, respectively, while azithromycin resistance was prevalent at 76.3%. Among newer antibiotics, colistin, fosfomycin, and nitrofurantoin resistance rates were 15.3%, 51.1%, and 39.2%, respectively.
The convergence of hypervirulence and antibiotic resistance in these strains presents a formidable challenge as traditional treatment options have become increasingly limited.
The meta-analysis also found a trend of increasing resistance to several antibiotics over time, significant differences in resistance across countries and regions, and variabilities in testing methods and standards.
The authors say global collaboration, standardized testing protocols, and tailored regional interventions will be needed effectively combat the threat of resistance in hvKp strains.
"This study serves as an urgent call for healthcare professionals, researchers, and policymakers to address this burgeoning public health challenge, and significantly contributes to the understanding of antibiotic resistance in hvKp strains, offering valuable insights for future research, clinical practice, and the development of public health policies," they wrote.











