- Worrying trends are already emerging regarding the rapid spread of infectious diseases in Gaza, owing to intensifying hostilities, intense overcrowding, and disruptions in healthcare, water, and sanitation, the World Health Organization (WHO) said today. Since mid October, 33,551 cases of diarrhea have been reported, more than half in young children, a steep rise compared to the 2,000 monthly cases typically reported in Gaza in the age-group over the past 2 years. Nearly 9,000 cases of scabies and lice have been reported, about 12,600 cases of rash, and nearly 55,000 upper respiratory infections, the group said. Other problems include disruptions in vaccination and disease surveillance and struggles to maintain infection prevention and control practices in healthcare facilities. The WHO repeated calls to ramp up humanitarian aid and for all parties in the conflict to abide by humanitarian law.
- In the latest US avian flu developments, Missouri reported an outbreak at a broiler breeder farm in Benton County that houses 16,600 birds, according to an update from the US Department of Agriculture (USDA) Animal and Plant Health Inspection Service (APHIS). Also, officials reported 21 more highly pathogenic H5N1 avian flu detections in wild birds, mostly from the Midwest and West. Species range from American white pelicans in Iowa to a few captive birds in Arizona.
- Florida reported 12 more locally acquired dengue infections, raising the year’s total to 110, the Florida Department of Health said in its latest update. Most cases this year were in Miami-Dade County, but a few other cases were in Broward, Hardee, Palm Beach, and Polk counties.
Quick takes: Worrying disease trends in Gaza, avian flu expansion, more dengue in Florida
VA hospitals more likely to use contact precautions for multidrug-resistant organisms

A cross-sectional survey of US hospitals found that Veterans Affairs (VA) hospitals were more likely to use contact precautions for patients with multidrug-resistant organisms than non-VA hospitals, researchers reported yesterday in the American Journal of Infection Control.
The survey, conducted from April 2021 to May 2022, was sent to 127 infection preventionists at all VA hospitals and 881 from a random sample of non-VA hospitals. Respondents were asked about hospital and infection control program characteristics and various infection transmission-focused prevention practices, such as hand hygiene and contact precautions (eg, use of gloves and gowns for contact with patients with a known or suspected infection). The overall response rate was 56% for VA hospitals and 47% for non-VA hospitals.
Greater use of contact precautions, supplemental cleaning devices
The mean reported hand hygiene compliance rate and percentage of hospitals using direct observation to monitor compliance was 90% among both the VA and non-VA hospitals, and roughly 60% of VA and non-VA hospitals reported use of the antiseptic chlorhexidine gluconate for daily bathing of intensive care unit patients.
But a higher percentage of VA versus non-VA hospitals reported using contact precautions with active surveillance culturing for methicillin-resistant Staphylococcus aureus (56.7% vs 24.4%) and carbapenem-resistant Enterobacterales (26.9% vs 13.3%) and for vancomycin-resistant Enterococcus without surveillance culturing (67.7% vs 38.9%).
In addition, a higher percentage of VA hospitals (67.6% vs 52.9%) reported using supplemental no-touch disinfection devices to clean rooms used to care for patients with Clostridioides difficile infection.
The study authors say the differences may be attributed in part to nationally coordinated VA initiatives related to transmission-based practices, as well as studies showing the efficacy of these practices in preventing disease transmission at VA hospitals.
US hospital safety group reports reduction in healthcare-associated infections
New data from a nonprofit hospital safety group show that many US hospitals have cut their rate of hospital-acquired infections (HAIs) over the past year.

The data from the latest Leapfrog Hospital Safety Grades show that over 85% of US hospitals have reduced the rate of at least one of the three HAIs monitored by the group—methicillin-resistant Staphylococcus aureus (MRSA), central-line associated bloodstream infections (CLABSIs), and catheter-associated urinary tract infections (CAUTIs)—since fall 2022. Nineteen percent of hospitals have reduced the rates of all three HAIs.
The report assigns a letter grade to nearly 3,000 US hospitals based on how well they prevent medical errors, accidents, and infections. Nearly 30% of the hospitals in this year's report received an "A" grade, 24% earned a "B," 39% received a "C," 7% earned a "D," and less than 1% received an "F."
Pandemic-related spike in HAIs
The reductions are noteworthy because Leapfrog's previous report, released in May, showed that HAIs hit a 5-year high at US hospitals during the COVID-19 pandemic, with the average standard infection ratios of MRSA and CLABSI climbing by 35% compared with prepandemic levels and CAUTIs rising by 20%.
That data mirrored findings from the Centers for Disease Control and Prevention on HAI spikes in hospitals in 12 states in 2020, adding to the growing body of evidence that the pandemic negatively affected infection prevention and control efforts in US hospitals. Prior to 2020, HAI rates at US hospitals had been declining.
"Now that we have pre- and post-pandemic data for patient safety measures, we are encouraged by the improvement in infections and applaud hospitals for reversing the disturbing infection spike we saw during the pandemic," Leah Binder, president and CEO of The Leapfrog Group, said in a press release.
Organ transplant patients on maintenance drugs at increased risk for COVID hospitalization

Maintenance immunosuppressive drugs, including steroids, used for organ transplant patients are associated with an increased risk of COVID-19 hospitalization in solid-organ transplant recipients, according to new findings.
The study, published yesterday in JAMA Network Open, was based on findings among a cohort of 60,456 solid-organ transplant recipients in France. The average age of participants was 59, and 63.7% were male. Patients were tracked from February 15, 2020, to July 31, 2022.
Among participants found in the French National Health Data System, 41,463 (68.6%) had kidney transplants, 14,464 (23.9%) had liver transplants, 5,327 (8.8%) had heart transplants, and 2,823 (4.6%) had lung transplants. Overall, 11.4% were hospitalized for COVID-19, including 12.7% of kidney transplant recipients, 6.4% of liver transplant recipients, 12.9% of heart transplant recipients, and 18.0% of lung transplant recipients.
Heart transplant patients at greatest risk
In kidney transplant recipients, steroids (adjusted odds ratio [AOR], 1.60; 95% confidence interval [CI], 1.49 to 1.73) and mycophenolic acid (AOR, 1.37; 95% CI, 1.25 to 1.51) were associated with a high risk of hospitalization.
Steroids were also associated with an increased risk of hospitalization for COVID-19.
"We observed an increased risk of COVID-19 hospitalization associated with using sirolimus in heart transplant recipients and using mycophenolic acid in kidney and liver transplant recipients independent of other drugs," the authors wrote. "Steroids were also associated with an increased risk of hospitalization for COVID-19 in each transplant subgroup."
Tacrolimus and cyclosporine were the only two maintenance therapies associated with a low risk of hospitalization in liver and heart transplant recipients, respectively.
Among all participants, heart transplant recipients treated with sirolimus were at the greatest increased risk of COVID-19 hospitalization (AOR, 2.71; 95% CI, 1.20 to 6.09).
Many mpox patients have other sexually transmitted infections, study shows
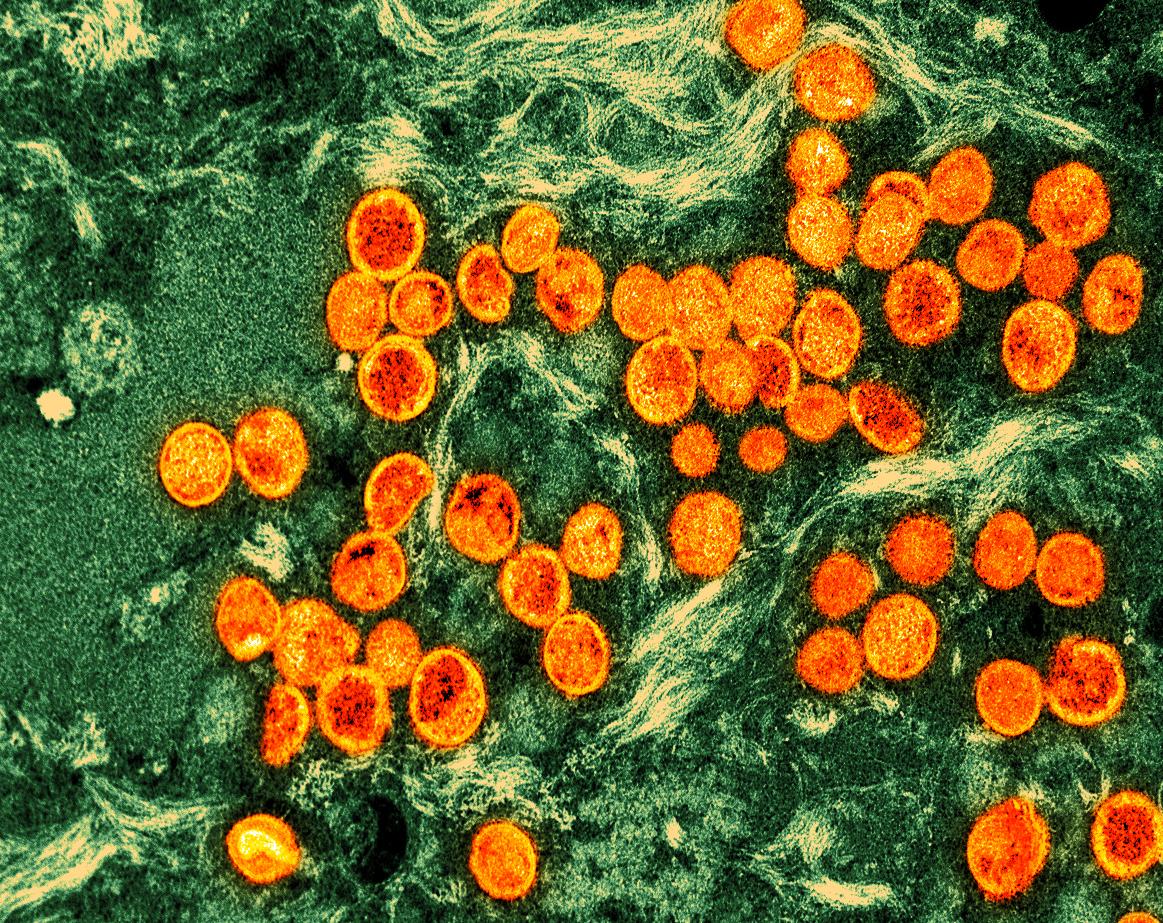
A large proportion of mpox patients in Chicago last year and early this year also had other sexually transmitted infections (STIs) such as HIV, predisposing them to severe mpox and potentially contributing to spread of the virus, finds a study led by Chicago Department of Public Health researchers.
The findings, published today in the Journal of Infectious Diseases, involved estimating rates of HIV and other STIs (in this case, gonorrhea and chlamydia) among 1,124 mpox patients from June 2022 to March 2023 and identifying factors tied to mpox severity. Median age was 34 years, 36% were White, 30% were Hispanic, 29% were Black, 92% were cisgender, and 83% of 806 who reported partner sex said they had a male partner.
A multicountry mpox outbreak began in nonendemic countries in May 2022, with most cases in men who have sex with men (MSM). Cases continue to be identified in Chicago, the researchers noted. Advanced HIV is tied to mpox-related hospital admissions and death, and those with weakened immune systems may be more likely to spread the virus to others.
Concurrent HIV tied to hospitalization, death
Of the 1,124 mpox patients, 44% had HIV, and 70% had a previous or current STI, with 39% having had at least three previous STI episodes. Relative to mpox patients who didn't have HIV, more HIV-infected mpox patients were hospitalized (10.3% vs 4.1%). A total of 76 (7%) of patients were hospitalized—66% of them HIV patients—and all 3 patients who died had advanced HIV.
STI screening visits are opportunities to vaccinate against mpox and provide HIV prophylaxis or treatment.
Of 335 vaccinated mpox patients, 55% had received one dose of the Jynneos vaccine, and 45% had received two. In total, 17.6% were vaccinated before mpox infection, and 2% had received two doses.
"STI screening visits are opportunities to vaccinate against mpox and provide HIV prophylaxis or treatment," the study authors wrote. "Future research should examine predictors of mpox infection among those with STIs, including other STIs, such as syphilis, HIV risk at STI screening or anatomical site of infection."











