Eleven deer tested positive for chronic wasting disease (CWD) in the 2022-23 hunting season in Tensas Parish, Louisiana, raising the state's total to 12 cases since the prion disease was first detected in the parish in January 2022, according to a notice from Louisiana Department of Wildlife & Fisheries (LDWF).
A total of 2,370 hunter-harvested deer in Louisiana were tested for CWD during the 2022-23 hunting season.
Deer in affected areas should be tested before eating
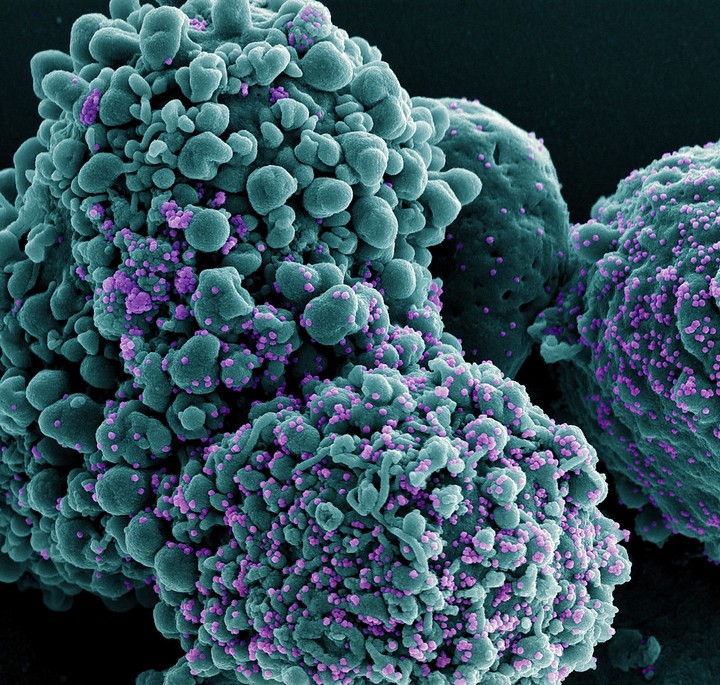
CWD is a fatal neurodegenerative disease affecting cervids such as white-tailed deer. The causative prion, a misfolded protein particle, is transmitted among deer via urine, feces, and carcasses. Infected deer may lose weight, drink water and urinate more than usual, salivate excessively, and display circling and a lack of coordination and fear of people.
CWD hasn't been found to spread to humans, but the US Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) recommend against consuming CWD-infected venison. Hunters in areas with a history of CWD should submit their deer for testing for the disease before eating the meat.
 Shielding, a public health strategy used across the United Kingdom in the early months of the pandemic, aimed to keep the most vulnerable citizens protected from the novel coronavirus at home and away from public-facing jobs and schools. But a new study of Welsh citizens published in the
Shielding, a public health strategy used across the United Kingdom in the early months of the pandemic, aimed to keep the most vulnerable citizens protected from the novel coronavirus at home and away from public-facing jobs and schools. But a new study of Welsh citizens published in the  An analysis of stool samples from patients in Mozambique, nearly half of whom had
An analysis of stool samples from patients in Mozambique, nearly half of whom had 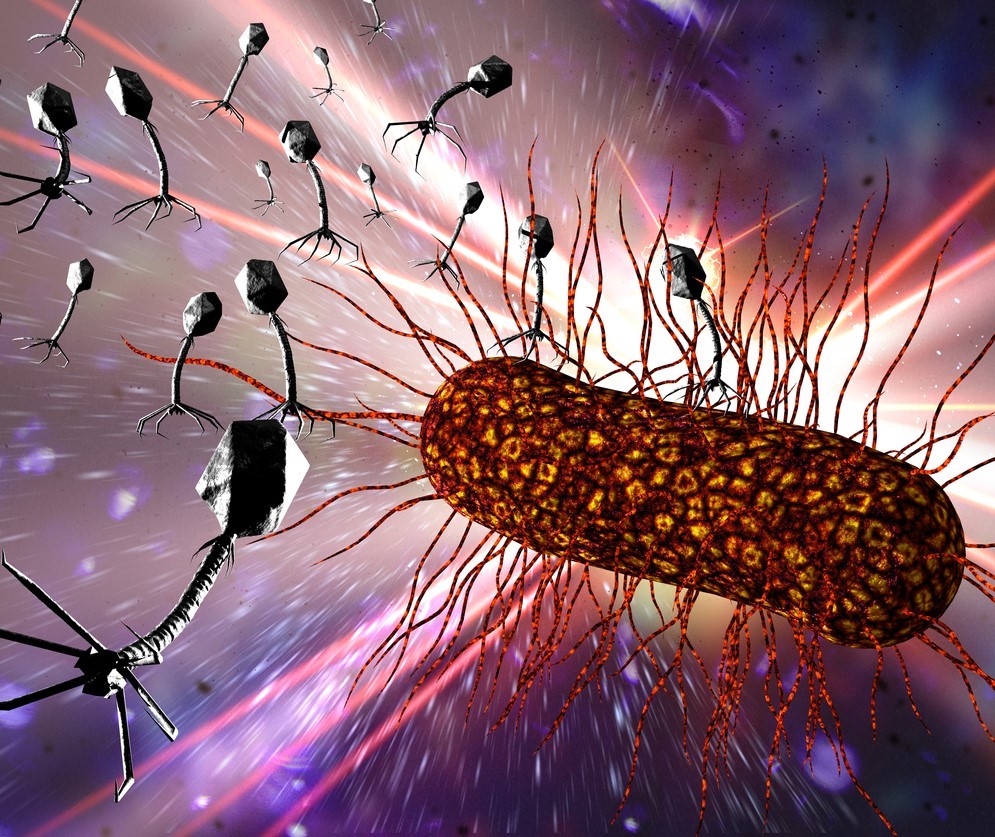 Researchers with the Israeli Phage Therapy Center (IPTC)
Researchers with the Israeli Phage Therapy Center (IPTC) 













