- Three mosquitoes out of more than 100 collected from Florida's Sarasota County—where four human cases were recently confirmed—were positive for the malaria parasite in testing at the Centers for Disease Control and Prevention (CDC), according to CBS News, which cited Sarasota County Mosquito Management Services. The finding was previously reported by the Sarasota Herald-Tribune. The mosquitoes that were positive were all from the same woodlot.
- Four African countries reported new polio cases this week, all involving vaccine-derived types, according to the latest weekly update from the Global Polio Eradication Initiative. The Democratic Republic of Congo reported four cases involving circulating vaccine-derived poliovirus type 1 (cVDPV1) and three that were due to circulating vaccine-derived poliovirus type 2 (cVDPV2). Madagascar reported three cVDPV1 cases, and Nigeria and Zambia reported three and one cVDPV2 cases, respectively.
- In an update yesterday the CDC reported one more death in the fungal meningitis outbreak linked to epidural anesthesia given at two Mexican cosmetic surgery clinics, raising the total to seven. So far, nine cases have been confirmed by fungus detected in spinal tap samples. The CDC also lists 15 cases as suspected and 10 as probable.
Quick takes: Dengue in Florida mosquitoes, polio in Africa, fungal meningitis deaths rise to 7
Paxlovid tied to 30% lower risk of severe COVID in patients with chronic conditions
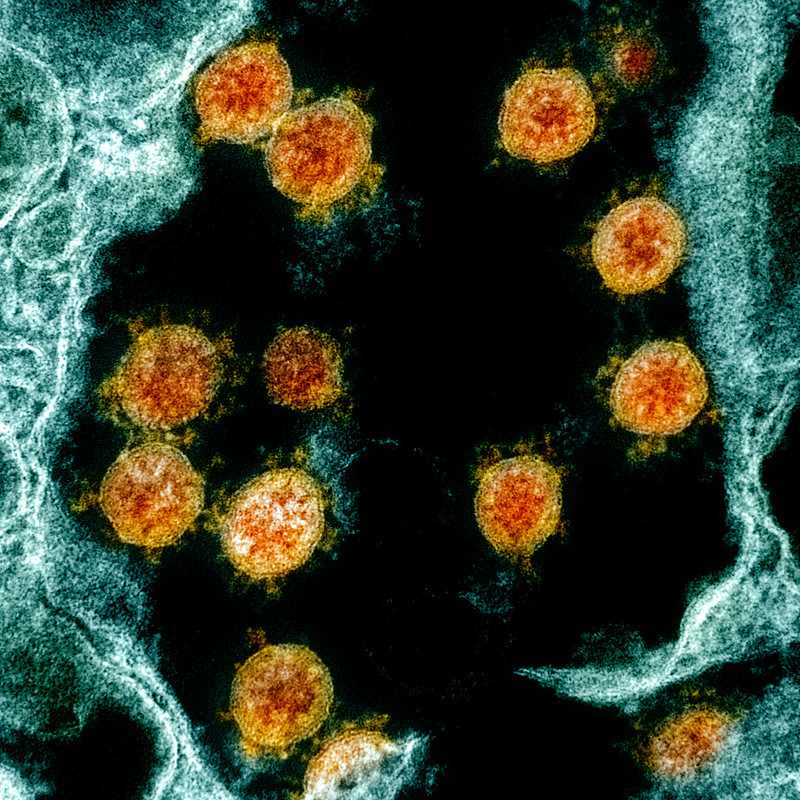
Paxlovid was linked to a 30% lower risk of all-cause emergency department (ED) visits, hospitalization, and death among vaccinated, nonhospitalized COVID-19 patients with serious chronic conditions but didn't appear to benefit those with only asthma or chronic obstructive pulmonary disease (COPD) or no serious underlying conditions, concludes a Harvard University–led study.
For the observational study, published today in Clinical Infectious Diseases, researchers assessed outcomes among two groups of 2,547 COVID-19 patients aged 18 to 50 years.
Participants had been vaccinated from December 2021 to July 2022, and the search was conducted in September. One group received Paxlovid (nirmatrelvir plus ritonavir), while the matched control group didn't.

5% vs 7% had poor outcomes
A total of 4.9% of Paxlovid recipients visited an ED, were hospitalized, or died in the first 30 days after COVID-19 onset, compared with 7.0% of controls (odds ratio [OR], 0.683), for a 30% reduction in relative risk. The number of patients needed to treat (NNT) to prevent one of these outcomes was 47.
Subgroup analyses revealed significant associations between Paxlovid benefit and patients with cancer (NNT, 45), cardiovascular disease (30), and both conditions (16). But no benefit was observed for patients with only chronic lower respiratory disorders such as asthma or COPD or without serious underlying illnesses.
Ten patients died, none of whom had received Paxlovid. There were no significant differences in rates of all-cause ED, clinic, or telehealth visits.
Paxlovid recipients had lower rates of constitutional, cardiovascular, and respiratory symptoms than controls, while rates of gastrointestinal, nervous, and musculoskeletal symptoms and altered smell or taste were comparable in both groups.
"The need for stewardship and more careful resource allocation are anticipated to increase, as decreases in government funding for Covid-19 treatments are expected," the researchers wrote. "Clinicians and policymakers should consider these findings, so that vital treatments are prescribed for those who need them (including those who have been underserved) and not wasted on those who stand to gain no benefit."
US COVID markers stay low
The indicators the Centers for Disease Control and Prevention (CDC) uses to track COVID activity remain low, according to yesterday's update. Nationally, hospital admission rates for COVID declined 5.3% over the past week, and deaths remained level. For hospitalizations, most counties remain in the green zone, except for a few in Iowa, Louisiana, Nebraska, Texas, Wisconsin, and Wyoming.
Early indicators, which include emergency department (ED) visits for COVID and test positivity, also remain low. ED visits for the virus declined 0.3%, with the percentage of weekly ED visits for COVID at just 0.5%. Nationally, COVID test positivity is 4.3%, up 0.1% over the past week. Positivity was slightly higher in the CDC region that includes California, the lower Midwest states, and the region that mainly includes New York, New Jersey, and Puerto Rico.
CDC director endorses RSV vaccine recommendation for older adults
Outgoing Centers for Disease Control and Prevention (CDC) Director Rochelle Walensky, MD, MPH, yesterday endorsed last week's Advisory Committee on Immunization Practices (ACIP) recommendation on use of two newly approved respiratory syncytial virus (RSV) vaccines in people ages 60 and older. The recommendation stipulates that people can get a single dose of the vaccine based on shared clinical decision making, meaning it isn't recommended for everyone in the age group.

The CDC said ACIP makes a shared clinical decision-making recommendation when individuals may benefit from vaccination, but broad vaccination isn't likely to have population-level impacts. Examples of other vaccines that have a shared clinical decision-making recommendation component include the meningococcal B vaccine for adolescents and young adults and the hepatitis B vaccine for adults age 60 and older who have diabetes. For such a recommendation, the CDC defines health provider as anyone who administers vaccines, including primary care physicians, specialists, physician assistants, nurse practitioners, registered nurses, and pharmacists.
The CDC said the vaccines are expected to be available this fall and that immunization provides an opportunity to protect older adults against severe RSV illness at a time when multiple respiratory viruses are expected to be circulating.
Review shows average mpox incubation period is 7 days, symptoms vary
A 21-study meta-analysis finds that the median incubation period for the global mpox outbreak that began last year is 7 days, symptoms vary widely, and immunocompromised people with HIV make up 36.1% of documented cases. The study is published in Archives of Virology.
This clinical review comes more than 1 year after countries around the world began seeing mpox as a sexually transmitted infection in communities that had never before seen the virus.
The studies included in the review described clinical presentation in 18,275 mpox cases. Most cases were caused by person-to-person transmission, and most infected men who have sex with men—the vast majority of patients—were young (30 to 40 years). Though the median incubation period—the time from exposure to symptom onset—was 7 days, the interquartile range was 3 to 21 days.
The clinical manifestations of mpox infection were severe skin lesions on the palms, oral, and anogenital regions, as well as proctitis, penile edema, tonsillitis, ocular disease, myalgia, lethargy, and sore throat. Unlike previous outbreaks of mpox, most patients do not experience a preceding fever before developing blisters.
Rash often first clue
"Instead, the illness often starts with a rash that appears as papules or blisters, which can be painful or itchy and progresses through several stages, forming crusts before healing," the authors wrote. Asymptomatic cases were also documented, but the study authors didn't specify how common they were.
Notably, the authors of the study said, hospitalizations, including admissions to intensive care units, have increased during the global outbreak. Among 84,470 cases reported since May of 2022, 80 deaths have been reported in 103 non-endemic countries.
Over 25% of kids in low-income nations receive antibiotics from unqualified sources
.jpg) An analysis of survey data from low- and middle-income countries (LMICs) found that roughly 1 in 4 children under the age of 5 received antibiotics from unqualified sources, researchers reported yesterday in eClinical Medicine.
An analysis of survey data from low- and middle-income countries (LMICs) found that roughly 1 in 4 children under the age of 5 received antibiotics from unqualified sources, researchers reported yesterday in eClinical Medicine.
To assess the proportion of antibiotics for children under 5 in LMICs that originated from unqualified sources (ie, without a prescription or medical supervision), researchers from Bangladesh used data from cross-sectional studies of the latest Demographic and Health Survey (DHS) datasets from 59 LMICs.
DHS is a global survey conducted every 3 to 5 years in LMICs that includes women between ages 15 and 49 and children under 5 who live in residential households. Among the items covered by the survey are illness and antibiotic use in children under 5.
The researchers identified 43,166 children under 5 who had taken an antibiotic for fever/cough 2 weeks prior to the survey, 74% of whom had obtained the antibiotic from a qualified source. The countries with the lowest percentage of antibiotics prescribed by qualified sources were Tanzania (22.4%), Bangladesh (23.7%), and the Democratic Republic of the Congo (46.2%). The countries with the highest percentage of antibiotics prescribed by a qualified source were Malawi (99.9%), Mozambique (96.3%), and Cambodia (94.7%).
In general, no subgroups were found to be especially high- or low-risk groups for taking antibiotics from qualified sources, but a higher percentage of children in rural areas (75%) received antibiotics from qualified sources compared with those in rural areas (72.2%), and the percentage of antibiotics received from qualified sources declined as the number of children under 5 in the household increased.
The study authors suggest that lack of access to medical treatment and lack of knowledge about antimicrobial resistance and inappropriate antibiotic use may play a role in obtaining antibiotics from unqualified sources.
"Our study calls for more robust health infrastructures and implementing various checks and balances for pharmacies not to provide antibiotics suggested by unqualified sources," they wrote. "The researchers hope this study will draw the attention of the relevant authorities to this appalling situation and recommend providing need-oriented support services at an individual level."
Study links multidrug-resistance, socioeconomic disparities
An analysis of bacterial isolates from hospitals in North Carolina and ZIP code-level socioeconomic data suggest that low-income status may be associated with higher levels of multidrug resistance, researchers reported today in Infection Control & Hospital Epidemiology.
For the study, a team of researchers from the University of North Carolina (UNC) and Duke University used microbiologic data and information from electronic health records to estimate the proportion of multidrug resistance in Enterobacterales isolates collected from patients in the UNC Health System from 2014 through 2021.
They then calculated the socioeconomic status (SES) subscore of the Social Vulnerability Index for each North Carolina ZIP code. The score represents the summed percentile ranking of a given ZIP code by five areas: poverty rate, unemployment rate, cost-burdened housing rate, percentage of residents who lack health insurance, and percentage of adults who lack a high-school diploma.
Of 90,129 isolates analyzed, 16,401 met the criteria for multidrug resistance, and 686 ZIP codes had 1 or more Enterobacterales-positive culture. The overall percentage of multidrug resistance was highest (19.9%) in the ZIP codes in the low SES quartile, and lowest in the high SES quartile (15.8%).
These findings indicate a need for further investigation into the disparities associated with [socioeconomic status] and infectious disease burden.
The prevalence ratios for multidrug resistance by SES quartiles, relative to the highest quartile, were 1.05 (95% confidence index [CI], 1.00 to 1.10) in the medium-high quartile, 1.24 (95% CI, 1.19 to 1.30) in the medium-low quartile, and 1.26 (95% CI, 1.20 to 1.31) in the lowest quartile. A similar pattern was observed in the relationship between SES and nonsusceptibility for individual antibiotic classes.
The study authors say the findings are consistent with past research suggesting that socioeconomic disadvantage is associated with higher disease burden. But the mechanisms behind the association remain incompletely defined.
"These findings indicate a need for further investigation into the disparities associated with SES and infectious disease burden," they concluded. "These data may help inform preventative efforts to decrease the burden of these important public health threats."











