Nov 7, 2011 (CIDRAP News) – A study billed as the largest to date of children who were critically ill with 2009 H1N1 influenza infections shows that neurologic conditions, immune problems, and methicillin-resistant Staphylococcus aureus (MRSA) coinfections increased their risk of dying.
The research, covering children treated in 35 US pediatric intensive care units (PICUs), showed that independent risk factors for death in children infected with the pandemic H1N1 (pH1N1) virus included female gender, preexisting neurologic conditions or immune compromise, early presumed MRSA coinfection of the lung, encephalitis, and myocarditis.
MRSA coinfections were the only independent risk factors in previously healthy children, according to the report, published online today in Pediatrics.
The researchers, with Adrienne G. Randolph, MD, of Children's Hospital Boston as first author, gathered data on patients with flu infections who were admitted to 35 PICUs in the Pediatric Acute Lung Injury and Sepsis Investigators' network of hospitals between April 2009 and April 2010. Data were gathered both retrospectively and prospectively.
They counted 838 patients, of whom 545 (65%) had pH1N1 confirmed by real-time polymerase china reaction or culture and 293 (35%) were classified as having probable pH1N1 on the basis of a positive test for influenza A without subtyping. Most of the children were identified prospectively, and 62% were admitted between September and November, during the peak of flu-related hospital admissions for the 2009-10 season.
The children's median age was 6 years, 58% of them were boys, and 70% had at least one chronic health condition. Most of the patients suffered respiratory failure, with 564 (67.3%) needing mechanical ventilation. Seventy-five children (8.9%) died.
Only 5.8% of the patients were on record as having received antiviral treatment before PICU admission, though 88.2% were treated with oral oseltamivir in the PICU. Extracorporeal membrane oxygenation (ECMO) was used in 33 patients (3.9%), of whom 61% died.
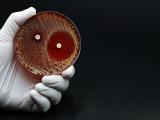
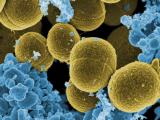
About a third of the children (274 of 838) had a clinical diagnosis of bacterial pneumonia or other evidence of bacterial coinfection within 72 hours of PICU admission. S aureus was identified in 26% (71 of 274) of these children, and 48% of these cases (34 of 71) involved MRSA. Pseudomonas species were the second most common type of bacterial infection found, at 11% (30 of 274 cases).
In multivariable analyses, the following conditions present at admission were found to be significant risk factors for death, with the percentages of patients affected, the relative risk (RR), and 95% confidence intervals (CI): female gender, 42.1%, 1.9 (1.2-3.0); a neurologic condition, 31.4%, 1.8 (1.1-2.7); immune compromise, 3.9%, 2.2 (1.1-4.5); encephalitis, 1.7%, 3.4 (1.6-7.5); myocarditis, 0.7%, 3.8 (1.2-12.0), and presumed MRSA lung coinfection within 72 hours, 41.%, 3.3 (1.7-6.4).
The 838 patients included 251 who were previously healthy. Of these, 26 had an early presumed S aureus lung infection, and this infection was present in 8 of the 18 previously healthy children who died. Six of these 8 cases involved MRSA. In the multivariable analysis, MRSA infection was found to be the only significant risk factor for death in the previously healthy patients (relative risk, 8; 95% CI, 3.1-20.6).
MRSA was not identified as a major pathogen linked to flu-related deaths in children before 2003, but several studies since then suggest that its role in severe flu complications in both children and adults has increased, the authors comment.
They note that previous research has found that neurologic disorders to be common in children who died from pH1N1 complications, but they say their study is the first to point to neurologic conditions as an independent risk factor for death. One previous study, from Korea, identified pH1N1-related myocarditis as an independent risk factor, they write.
The authors also note that most of the children who were coinfected with MRSA and died received vancomycin treatment promptly on admission to the PICU or earlier. This finding shows that improved strategies for preventing and treating influenza and related MRSA infections in children are urgently needed, they comment.
Randolph AG, Vaughn F, Sullivan R, et al. Critically ill children during the 2009-2010 influenza pandemic in the United States. Pediatrics 2011 December;128(6) (early online publication) [Abstract]