Our weekly wrap-up of antimicrobial stewardship & antimicrobial resistance scans
Metrics developed for assessing antimicrobial stewardship impact
A panel of experts has identified six metrics that hospitals can use to assess the impact of antimicrobial stewardship programs (ASPs).
In a Dec 7 paper in Clinical Infectious Diseases, researchers from Duke University and the Centers for Disease Control and Prevention (CDC) describe an effort to select relevant metrics that are both useful for assessing the impact of patient-level antimicrobial stewardship interventions and feasible to measure in acute-care hospitals. These metrics have been poorly defined for many reasons, the authors write, but mainly because care of patients with suspected infections is complex and analyzing suitable metrics is difficult and time consuming.
To come up with a consensus on a list of metrics, the researchers assembled a task force that included adult and pediatric infectious disease physicians and pharmacists with expertise in stewardship, along with healthcare epidemiologists, academic researchers, Veteran's Affairs representatives, and CDC stewardship experts. This panel evaluated a preliminary list of 90 metrics compiled from a review of published literature using a nine-point Likert scale, based on whether the metric is:
- Associated with improved antimicrobial prescribing
- Associated with improved patient care
- Useful in targeting antimicrobial stewardship efforts
- Feasible to monitor in any hospital with an electronic medical record
After two rounds of surveys and two teleconferences, the panel came up with a list of six metrics that the experts rated higher than 6 in all criteria: two metrics capturing the incidence of Clostridium difficile infection, incidence of drug-resistant infection, two measures of antimicrobial use, and one process measure (redundant therapy events). The panel also identified 14 metrics that scored well on all criteria except for feasibility.
"The selected measures align well with national priorities in improving and measuring antibiotic use and preventing drug resistance," the authors write, adding that measurement will soon be a required task under the Joint Commission antibiotic stewardship accreditation standard and the Centers for Medicare & Medicaid Services proposed antibiotic stewardship condition of participation.
"The metrics identified by this panel form a core set of measures that ASPs can start using immediately to both meet the measurement requirements and, more importantly, assess the impact of their efforts," the authors write.
Dec 7 Clin Infect Dis paper
Study finds post-prescription authorization may hold stewardship edge
Using a post-prescription review with feedback (PPRF) approach to antibiotic stewardship appears to be a bit more effective than employing pre-prescription authorization (PPA), according to a new Clinical Infectious Diseases study that measured the two strategies head to head at Johns Hopkins Hospital in Baltimore.
In the 8-month crossover trial, two medical teams were assigned to the PPA arm and two to the PPRF arm for the first 4 months of the study. The teams then switched to the other approach for the next 4 months. The study was conducted from September 2013 to June 2014 and involved about 2,700 patients using each approach.
The researchers found that antibiotic days of therapy (DOTs) remained relatively unchanged in the PPA arm. But when teams were switched to the PPRF arm, antibiotic use dropped 2.45 DOTs per 1,000 patient-days. For the teams that first used PPRF, antibiotic use decreased with that method 5.73 DOTs per 1,000 patient-days but did not change when those teams switched to the PPA method. Median patient DOTs in the PPA and PPRF arms were 8 and 6 per 1,000 patient-days, respectively (P = 0.03).
The authors concluded, "Both of these approaches are useful and impactful antibiotic stewardship techniques, but they both also require significant personnel time. We favor incorporating a combination of PPA and PPRF into stewardship activities but in settings where resources are limited precluding this possibility, our findings suggest it may be of more value to prioritize PPRF."
Dec 7 Clin Infect Dis abstract
Daily chlorhexidine bathing may cut MRSA, VRE
Daily bathing of patients with chlorhexidine gluconate (CHG) appears to reduce hospital-related methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE), according to a study yesterday in the American Journal of Infection Control.
Investigators in Vancouver conducted a prospective crossover study on four medical units that each contained 25 beds and were separated from each other from May 1, 2014, to Aug 10, 2015. Half the patients were bathed daily with no-rinse CHG cloths for 7 months, while the control group received soap-and-water baths. Each cohort involved more than 17,500 patient-days. Compliance with daily CHG bathing was 58%.
Hospital-associated MRSA decreased 55% (5.1 vs 11.4 cases per 10,000 inpatient days, P = .04) and VRE dropped 36% (23.2 vs 36.0 cases per 10,000 inpatient days, P = .03), respectively, compared with control patients. There was no significant difference in rates of hospital-associated C difficile.
The authors caution, however, "The success of CHG cloths in preventing infections relies on high compliance rates, both in routine use and in appropriate application of the product to the patient's skin. Before CHG is systematically implemented in health care facilities, extensive evaluation and discussion should be conducted with stakeholders. In the absence of unit and staff engagement, the anticipated benefits of CHG may not be realized."
Dec 8 Am J Infect Control study
Study finds link between drug resistance, early death in TB meningitis
Originally published by CIDRAP News Dec 8.
A study yesterday in Clinical Infectious Diseases reports an independent association between drug resistance and early mortality in patients with tuberculosis meningitis (TBM).
The study looked at a cohort of patients reported to the TB registry in New York City from 1992 to 2001, with a focus on patients with culture-confirmed TBM and reported susceptibility results for isoniazid and rifampin—the two frontline antibiotics for treating TB. Among the 360 patients who met those criteria, 324 initiated treatment with anti-TB drugs.
Of the 324 patients who initiated anti-TB therapy, 183 (56.5%) died before completing therapy, after a median survival of less than a month. Among 67 patients with rifampin-resistant isolates, 63 died before completion of therapy after a median of 31 days. But because 95% of these patients also had HIV, the investigators were unable to estimate the independent associations of HIV infection and rifampin resistance with mortality.
When controlling for age and HIV status, however, the researchers observed that, among the 257 TBM patients without rifampin-resistant isolates, isoniazid resistance was independently associated with mortality after the first 60 days of treatment.
"These findings support the continued evaluation of rapid diagnostic techniques and the empiric addition of second-line drugs for patients with clinically suspected drug-resistant TBM," the authors write.
Dec 7 Clin Infect Dis study
New drug-resistant Candida auris infections reported in Colombia
Originally published by CIDRAP News Dec 6.
Researchers in Colombia yesterday reported 17 originally misclassified cases of an emerging multidrug-resistant yeast, including at least 6 fatal cases.
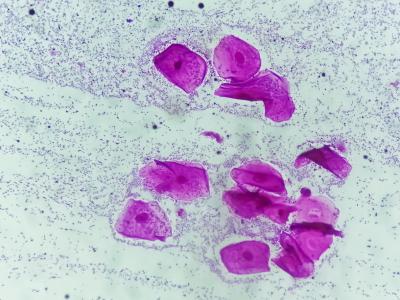
In a letter in Emerging Infectious Diseases, the researchers reported that 17 clinical isolates of Candida auris were recovered from 17 patients in 6 hospitals in northern Colombia from February through July 2016. C auris is a yeast that was first identified in a Japanese patient with an ear infection in 2009 and has since been reported in several other countries, including the United States. It has most commonly caused healthcare-associated invasive infections such as bloodstream infections, wound infections, and ear infections and has been associated with high mortality.
Of the 17 patients, 13 had fungemia (yeast in the blood). In the other 4 patients, C auris was isolated from peritoneal fluid, cerebrospinal fluid, bone, or urine. Most patients required a central venous catheter, a urinary catheter, and mechanical ventilation. The 30-day mortality rate in all patients was 35.2% (6 deaths); in those with fungemia, it was 38.4% (5 deaths).
One of the major concerns about C auris is that clinical isolates in several countries have shown varying levels of resistance to all three major classes of antifungal medicines used to treat Candida infections—including azoles, echinocandins, and polyenes. Another is that it is difficult to identify using common biochemical methods and is often misidentified as another type of Candida infection, which could lead to improper treatment.
In the reported cases, the authors write that the infections were originally misidentified as C haemulonii, C famata, C albicans, or C tropicalis. Correct identification was 27.5 days after hospitalization, on average. No categorical interpretation of antifungal susceptibility results was available from the lab that tested the patients' samples.
Dec 5 Emerg Infect Dis letter
Study documents country variations in pediatric antibiotic prescribing
Originally published by CIDRAP News Dec 5.
An analysis of antibiotic prescribing in outpatient pediatric settings in three European countries—Italy, the Netherlands, and the United Kingdom—showed varied usage patterns that might be helpful for evaluating and modifying current antibiotic stewardship programs, according to a study in the latest issue of the Pediatric Infectious Disease Journal.
Researchers based their retrospective cohort study on prescribing information from electronic health records from 2001 to 2010, covering more than 2 million children. The databases include records for Italian children up to age 14 and for the Netherlands and the United Kingdom up to age 18. The team also looked at two newly proposed pediatric-specific quality indicators: the proportion of amoxicillin users (amoxicillin index) and the ratio between amoxicillin and broad-spectrum antibiotics (A/B ratio).
For all three countries, antibiotic use was highest in the first years of life.
Prevalence of antibiotic prescribing was highest in Italy at 52.0%, followed by the United Kingdom at 36.2%, and the Netherlands at 18.0%. UK clinicians showed a slight reduction in global and amoxicillin use over time, with low prescribing of broad-spectrum antibiotics. In the Netherlands, antibiotic prescribing is low and stable, but levels of broad-spectrum antibiotics are progressively increasing. Meanwhile, in Italian pediatric settings, patterns were dominated by broad-spectrum antibiotics.
The investigators noted that two pediatric quality indicators easily showed the patterns and that the total antibiotic prevalence indicators may both be useful for gauging national programs and making future improvements.
December Pediatr Infect Dis J abstract
Study: MDR-TB in Shanghai gaining resistance as it spreads
Originally published by CIDRAP News Dec 5.
A study in The Lancet Infectious Diseases indicates that multidrug-resistant tuberculosis (MDR-TB) strains in the largest city in China are largely being transmitted from person to person, and that many of those strains are becoming more resistant during transmission.
In the population-based, retrospective observational study, Chinese researchers performed genotyping and whole-genome sequencing of isolates from 7,892 patients in Shanghai who tested positive for TB from 2009 to 2012. They also measured strain diversity within and between genomically clustered isolates. The authors of the study say it's the first population-based study to combine genomics with detailed epidemiologic data to identify MDR-TB transmission pathways in a region in China, the country with the second-most MDR-TB cases worldwide.
It is commonly believed, the authors note, that most cases of MDR-TB result from inadequate treatment. But while many cases of MDR-TB strains are due to person-to-person transmission of MDR strains, few studies have provided evidence of transmission of MDR-TB at the population level. Understanding the causes and transmission patterns of MDR-TB is considered crucial for efforts to reduce the disease.
The findings suggest that transmission is common. Overall, the researchers found that 367 of the 7,892 patients (5%) had MDR-TB. They also found that nearly a third of the 324 MDR strains identified were in 38 genomic clusters that differed by 12 or fewer single nucleotide polymorphisms, which indicates recent transmission, and that transmission of MDR strains accounted for 73% of MDR-TB cases overall. Residential communities and related public facilities were the most common transmission settings.
Furthermore, transmission network analysis showed that 87% of the clusters acquired additional drug-resistance mutations during transmission.
"Transmission of MDR strains of tuberculosis has a substantial role in the burden of MDR tuberculosis in China," the authors write. "Interventions, such as early detection of cases, infection control, and evidence-based treatment, are urgently needed to stem the epidemic."
Dec 2 Lancet Infect Dis study