Two new MERS cases reported in Saudi Arabia
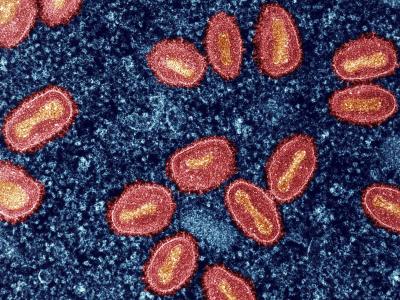
The Saudi Arabian Ministry of Health (MOH) updated its MERS-CoV statistics for the first time in more than a week, noting two new cases not related to current hospital outbreaks in Riyadh.
On Jun 22, the MOH said an 85-year-old Saudi man from Yanbu died from MERS-CoV (Middle East respiratory syndrome coronavirus). The source of infection was listed as "primary," meaning it's unlikely he contracted the disease from another person.
Yesterday, the MOH said a 30-year-old Saudi woman from Dammam was in critical condition after presenting with symptoms of MERS-CoV. She had indirect contact with camels, a known risk factor for the coronavirus. Neither patient is a healthcare worker.
The new cases bring Saudi Arabia's MERS-CoV cases since 2012 total 1,667, including 680 deaths. Thirteen people are still being treated for their infections.
Jun 22 MOH report
Jun 25 MOH report
WHO: Flu continues slow rise in Southern Hemisphere countries
Flu activity in the Southern Hemisphere continues to increase and has passed the seasonal threshold in some South American countries such as Chile and Paraguay, where H3N2 is the dominant strain, the World Health Organization (WHO) said today in a global flu update, which includes activity through Jun 11.
In more tropical areas of South America, flu activity remained low, with a slight increase in Brazil that is still below the alert level. In Australia and New Zealand, flu has increased from baseline to average levels, with the region experiencing a mix of influenza A and B. Southern Africa is also reporting a rise in flu activity, with H3N2 as the predominant strain.
A few other regions of the world reported increasing flu levels, including the East African nations of Madagascar and Mauritius, as well as Hong Kong, where H3N2 is the main strain and Vietnam, where 2009 H1N1 and influenza B are predominant. Also, a few West Asian nations including Oman and Qatar reported slight increases.
At the global level, among recent specimens that tested positive for flu, 68.2% were influenza A and 31.8% were influenza B. Of the subtyped influenza A viruses, 68.5% were H3N2.
Jun 26 WHO global flu update
New study details pediatric symptoms of Lyme disease
A new study presented at the Pediatric Academic Societies meeting described the range of symptoms associated with Lyme disease in children, in an effort to help providers understand what can be expected after a course of antibiotic treatment for the tick-borne disease.
Prompt treatment with antibiotics is considered the gold-standard for Lyme disease. Most symptoms develop after a tick has been attached to a child for 36 or more hours—enough time to sufficiently transmit the Lyme disease spirochete. The "bulls-eye" rash, which occurs with most but not all infections, usually appears within 7 to 10 days of a bite. Fever, body aches, headache, and musculoskeletal pain are all known symptoms of Lyme.
The study was based on the electronic medical records of 79 children admitted to the Children's National Health System with laboratory-confirmed diagnosis of Lyme disease from June 2008 to May 2015. The researchers looked at how long certain symptoms lasted, including headache (usually present at disease onset) and knee pain (apparent weeks after diagnosis). Headaches tended to dissipate within 3 days of antibiotic treatment and did not return, no matter how long a child had been reporting them before beginning antibiotic therapy. Knee pain, however, took 2 to 4 weeks to resolve.
Only 2 of the 79 children included in the study had symptoms 6 months after diagnosis, a phenomenon known as post-treatment Lyme disease syndrome.
Jun 26 Children's National Health System press release