Scientists conducting an observational cohort study in an ongoing mpox outbreak in the Democratic Republic of the Congo (DRC), which involves a different clade than the global outbreak, have identified a possible third route of mpox transmission: sexual activity involving heterosexuals.
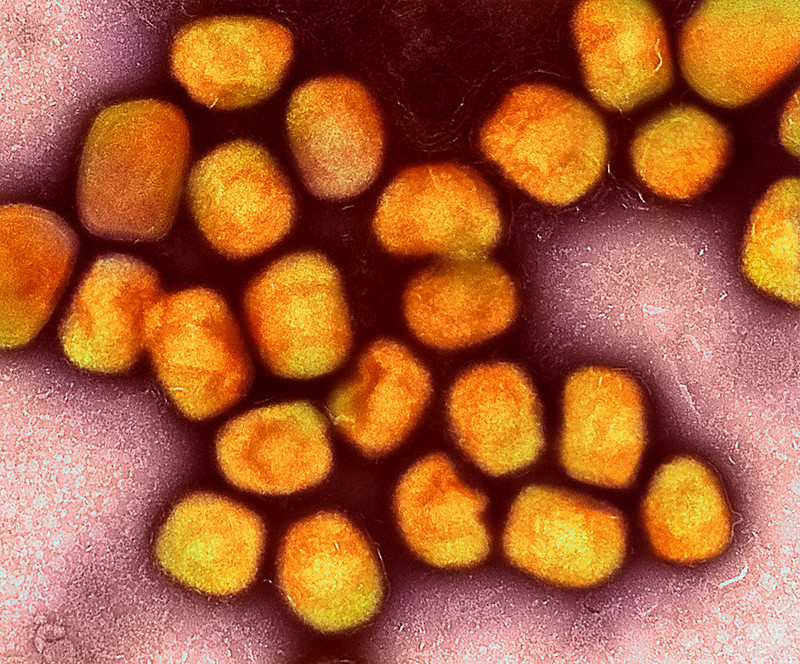
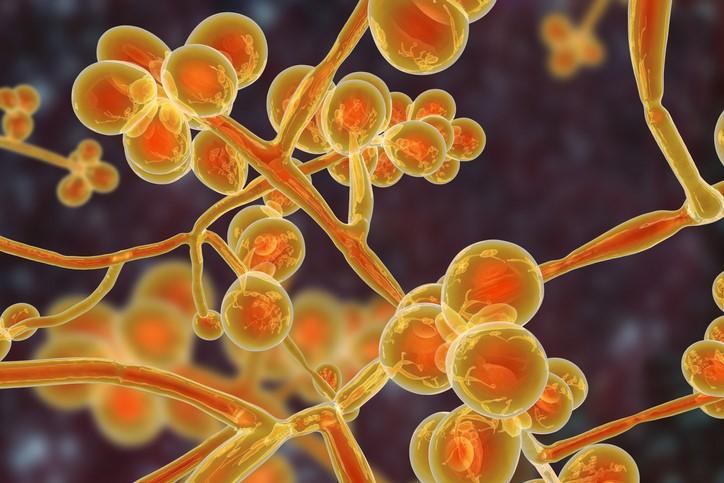
An outbreak in the DRC's South Kivu province has been under way since August 2023. The outbreak is centered in Kamituga, and scientists have identified a distinct clade 1 mpox strain, which may be a novel subgroup. An international research team published its findings this week in medRxiv, a preprint server hosting studies that are not yet peer-reviewed.
So far, more than 200 mpox cases have been reported in the Kamituga area.
The outbreak made headlines in in late 2023, because it was the first known clade 1 outbreak fueled by sexual transmission. Typically, clade 1 infections involve zoonotic spillovers with some human-to-human spread. Clade 1 infections are known to be more virulent and deadly, with case-fatality rates as high as 10%.
Female sex workers main occupational group
For the study, researchers interviewed 51 of 164 patients who were admitted to Kamituga hospital September 2023 through January 2024. Of that group, 24 were professional sex workers. The most common symptoms were fever and oral and anogenital lesions. Two deaths were reported.
Heterosexual partners were mainly affected, suggesting that heterosexual contact may be the main form of transmission. The investigators wrote that professional sex workers –primarily young women–were the dominant occupational group, suggesting that they and their clients may be at higher risk for contracting mpox.
So far, there's no sign that clade 1 is spreading outside of central Africa, the European Centre for Disease Prevention and Control said in a December risk assessment.