Researchers report that immunity against pertussis (whooping cough) was sustained 5 years after receipt of a recombinant vaccine in adolescents and young adults, a finding that they said supports its use as a booster in adolescents.
The study was a follow-up of participants vaccinated 5 years earlier, at ages 12 to 17 years, with recombinant acellular pertussis vaccine during a phase 2/3 randomized clinical trial conducted from July 2015 to November 2016 in Thailand. Participants had received three doses of whole-cell pertussis vaccine as infants.
Of 159 participants, 55 received the pertussis-only vaccine formulation (aPgen), 52 received tetanus-diphtheria-pertussis (TdaPgen), and 52 received the Tdapchem booster.
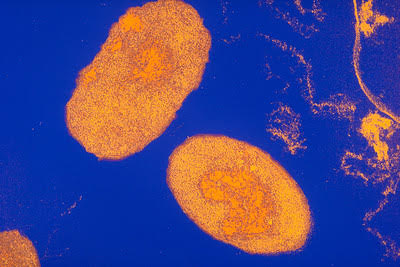
The team collected a blood sample and measured serum PT-immunoglobulin G (IgG) and filamentous hemagglutinin (FHA)-IgG antibody levels in all participants and pertussis toxin (PT) neutralizing antibody titers in the 55 aPgen recipients. Antibody concentrations were analyzed with enzyme-linked immunosorbent assay (ELISA) and Chinese hamster ovary assays.
"Pertussis toxin (PT), particularly if genetically detoxified (PTgen), represents the main antigen ensuring protection from pertussis disease," the authors wrote. "We previously demonstrated that recombinant acellular pertussis vaccines containing PTgen are more immunogenic and induce significantly higher PT-neutralizing antibody titers in adolescents than chemically inactivated tetanus-diphtheria-pertussis booster vaccines (Tdapchem)."
The results were published today in JAMA Network Open.
Results support use as boosters in teens, adults
Five years post-vaccination, levels of neutralizing anti-PT antibodies were more than fourfold greater than the seropositivity cutoff of 5 international units per milliliter (IU/mL). PT neutralizing antibody concentrations were 2.5-fold (aPgen) and threefold (TdaPgen) higher than prevaccination. PT-IgG antibody levels were greater than 20 IU/mL in 75% of aPgen vaccine recipients and 56% of TdaPgen recipients, compared with 27% of Tdapchem recipients.
"Long-lasting protection was demonstrated earlier in an efficacy trial for PTgen-containing [genetically detoxified] recombinant vaccines after primary immunization in infants," the authors wrote. "Our findings suggest that PTgen-containing vaccines can also offer longer-lasting protection in adolescents, supporting their use as booster vaccines in adolescents and adults to enhance population immunity.
.jpg)
.jpg)












