More countries in Africa and the Middle East reported new polio cases, all involving vaccine-derived strains, according to updates from the Global Polio Eradication Initiative (GPEI) and Israel's health ministry.
African countries reporting more circulating vaccine-derived poliovirus type 2 cases include Benin (1), Cameroon (1), the Democratic Republic of the Congo (DRC; 8 cases), Mali (1), and Somalia (1). Also, two countries in the region reported more circulating vaccine-derived poliovirus type 1 (cVDPV1) cases: the Republic of Congo (1), its first involving the strain, and the DRC (13).
In the Middle East, Yemen reported one cVDPV2 case. Also, Israel's health ministry recently reported an illness in an unvaccinated 8-year-girl from Safed, a city in Israel's Northern District. On Twitter, the health ministry said the epidemiologic investigation into the girl's illness has turned up three positive cases in asymptomatic children who were listed as contacts. The health ministry said sewage sampling continues to find positive samples from many of the country's settlements and that 150,000 children are unvaccinated.
Last year, Israel reported its first polio infection in more than 30 years, in a child who was infected with circulating vaccine-derived poliovirus type 3 (cVDPV3). Also, vaccine-derived poliovirus type 2 was detected last year in wastewater samples from Jerusalem.
 Although bacterial co-infections were identified infrequently in hospitalized US COVID-19 patients, they were associated with a more than two-fold higher risk of death, US researchers
Although bacterial co-infections were identified infrequently in hospitalized US COVID-19 patients, they were associated with a more than two-fold higher risk of death, US researchers 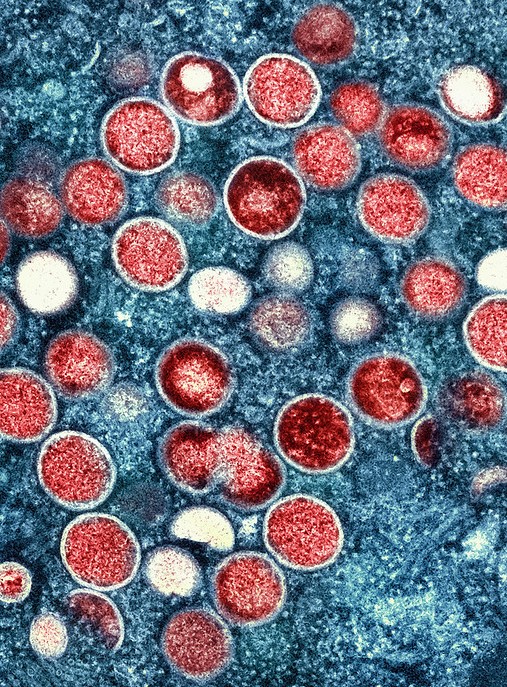 The average time for symptom onset between successive mpox cases (serial interval) is 8.5 days, and the average time between infection and symptom onset (incubation period) is 5.6 days, estimates a
The average time for symptom onset between successive mpox cases (serial interval) is 8.5 days, and the average time between infection and symptom onset (incubation period) is 5.6 days, estimates a 











