- The US Department of Agriculture (USDA) Animal and Plant Health Inspection Service (APHIS) confirmed one more H5N1 avian flu outbreak in dairy cattle, another from California. The outbreak brings the national total since the outbreaks began in March to 243 across 14 states. California, the nation’s largest dairy producer, has now reported 44 outbreaks since late August.
- The California Department of Public Health (CDPH) today urged residents to take precautions following an increase in diseases caused by mosquitoes. So far, the state has reported 63 human cases of West Nile virus, 6 of them fatal, from many of the state’s regions but especially the Central Valley. Also, it noted four dengue infections reported from Los Angeles County, including three that are part of a cluster from Baldwin Park. The CDPH urged people to protect themselves from mosquito bites and get rid of standing water where mosquitoes breed.
- Gavi, the Vaccine Alliance, today released a report on its 2023 activities, estimating that the vaccine programs it supported last year will prevent 1.3 million deaths. It said 69 million children were immunized, the second highest in one year. The group said another achievement was a big increase in its human papillomavirus vaccination program, which saw 14 million girls immunized, a number greater than the previous 10 years combined.
Quick takes: More H5N1 in dairy cows, mosquito-borne illnesses in California, Gavi vaccine impact
Study: COVID-19 vaccination protects against serious cardiovascular disease
Full vaccination against COVID-19 protects recipients from serious cardiovascular disease linked to COVID-19, according to a new study in the European Heart Journal.
The findings come from a review of more than 8 million adults in Sweden who were followed up in national healthcare registers from the end of December 2020—when COVID-19 vaccination began—until the end of 2022.
Among the 8,070,674 adults included in the study, 88.5% received at least one dose of vaccine, 86.9% at least two, and 67.9% three or more. There were 1,668,508 new cases of COVID-19; 40.3% occurred before the first dose of vaccination, 3.7% between the first and second dose, 34.3% between the second and third dose, and 21.7% after the third dose.
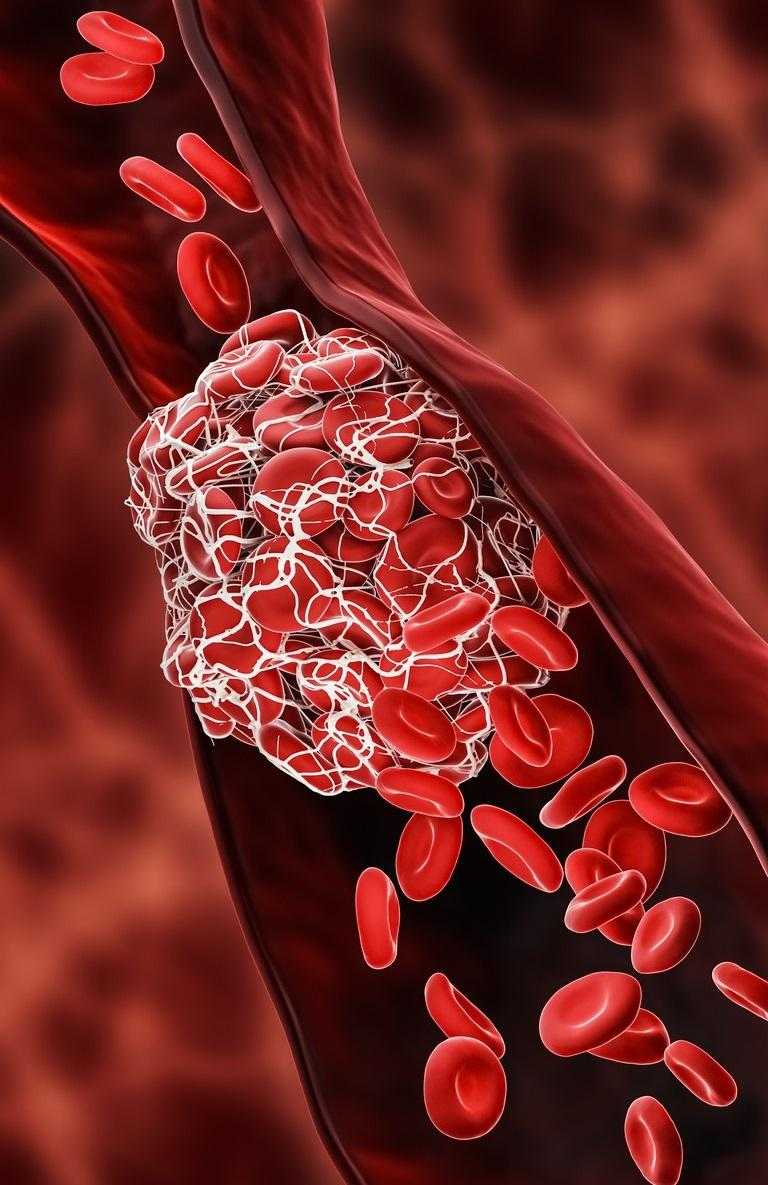
Outcomes included inflammation of the cardiac muscle or the pericardium, cardiac arrhythmia, heart failure, transient ischemic attack (TIA), and stroke.
Individual vaccine doses linked to increased risk
Overall, vaccination was associated with decreased risks of cardiovascular disease by about 20% to 30% compared to no vaccination.
The authors note, however, that some cardiovascular effects have been seen after individual doses of the vaccine, especially among older men.
There was a 17% higher risk of extrasystoles, or extra heart beats, after dose one and 22% after dose two. While the overall the risk of stroke was lower in vaccinated people, there was an increased risk of TIA.
"It should be noted that for outcomes showing slightly increased risks (myopericarditis, TIA, and extrasystoles), the incidence rates were generally lower than for the other outcomes that showed decreased risks," the authors said.
The increases in cardiovascular risk we saw following COVID-19 vaccination are temporary, and do not apply to the more severe conditions
"The increases in cardiovascular risk we saw following COVID-19 vaccination are temporary, and do not apply to the more severe conditions," said study author Fredrik Nyberg, PhD, in a press release from the University of Gothenburg. "On the other hand, full vaccination significantly reduced the risk of several more severe cardiovascular outcomes linked to COVID-19, such as heart attack, stroke, and heart failure. This emphasizes the protective benefits of full vaccination."
Study provides novel insights on sepsis in India

A study conducted in southern India found that sepsis disproportionately affects younger and mostly rural groups and that gram-negative bacteria, viruses, and tropical diseases are significant causes, researchers reported today in Clinical Infectious Diseases.
To gain insight into the causative agents and characteristics of patients with community-acquired sepsis in India, which accounts for 26% of global sepsis-related deaths, a team of researchers from India, the Netherlands, and the United Kingdom conducted a prospective observational study in a tertiary-care hospital in South India from December 2018 through September 2022. They enrolled adult patients within 24 hours of intensive care unit admission (ICU) who met international sepsis criteria and collected clinical, microbiologic, demographic, and outcome data.
Of the 4,000 patients screened on ICU admission, 1,000 (median age, 55 years; 66% male) met the inclusion criteria. Most patients lived outside of urban areas, with 23.7% living in towns and 46.5% in villages, while roughly half had no formal education, and three-quarters worked in the primary sector. The median length of ICU stay was 4 days, and in-hospital mortality was 24.1%.
Study fills important knowledge gaps
A causative agent could be identified in 54% of patients, with bacteria causing 38% of cases, viruses 18%, leptospirosis 10.6%, scrub typhus 4.1%, dengue 3.7%, and Kyasanur forest disease virus (KFDV) 1.6%. Sepsis cases caused by leptospirosis, scrub typhus, dengue, and KFDV all showed seasonal variation around the monsoon season.
Among patients with bacterial sepsis, 43.9% of isolates were gram-negative; Escherichia coli (52.3%), Klebsiella pneumoniae (23.3%), and Pseudomonas aeruginosa (5.3%) were the most frequently isolated species. Further analysis found high levels of antibiotic resistance, with 75.8% of E coli, 47.7% of K pneumoniae, and 30% of P aeruginosa resistant to third-generation cephalosporins and 10.1%, 13.6%, and 10.0% resistant to carbapenems, respectively.
"This study provides a detailed examination of sepsis in South India and fills important knowledge gaps of the real burden of sepsis in LMICs [low- and middle-income countries]," the study authors wrote. "These findings provide critical groundwork for strengthening capacity, optimizing resource allocation, and formulating evidence-based treatment guidelines specifically tailored to South Asia, underscoring the importance of regional epidemiologic sepsis research in LMICs."
UK supermarkets lack robust antibiotic policies, report finds

A new report reveals that UK supermarkets don't have strong enough policies to enforce new national legislation on antibiotic use on farms.
The legislation, which was enacted May 17, bans UK farmers from using antibiotics routinely and prohibits the use of antibiotics to "compensate for poor hygiene, inadequate animal husbandry, or poor farm management practices." But in a report released last week, the Alliance to Save Our Antibiotics found that 10 leading UK supermarket chains are failing to ensure that their suppliers are fully compliant with the new legislation.
For example, the report found that supermarket antibiotic policies still only apply to store-brand products and don't cover branded products or imported meat, fish, dairy, or eggs that may be produced with routine antibiotic use.
"The scope of the policies needs to be extended to branded foods and to imported food in order to protect consumers and ensure that British farming standards are not undermined by imports," the report states.
Supermarkets need to take 'strong and urgent' action
The report also found that only five of the chains publish good or acceptable data on the use of antibiotics in their supply chains, and only two have a full ban on the use of the last-resort antibiotic colistin. In addition, most of the chains continue to sell fast-growing breeds of broiler chickens that require more antibiotic use.
The group says that while UK supermarkets have made improvements since they published their first assessment in 2017 and have contributed to a 59% reduction in total farm antibiotic use since 2014, the new report indicates they have more work to do.
"It is no longer legal to use antibiotics to prop up farming methods that are causing animals to fall sick," Coilin Nunan, policy and science manager for the Alliance to Save Our Antibiotics, said in a press release. "So to avoid misusing antibiotics, and to keep animals healthy, supermarkets must now take strong and urgent action to improve animal husbandry and welfare."
In a statement, the Food Industry Initiative on Antimicrobials called the report misleading and said UK retailers' support for more responsible antibiotic use in their supply chains has played an integral role in reducing antibiotic sales and antimicrobial resistance on farms.











