Mar 28, 2012
ECDC: Climate change may promote Campylobacter, Salmonella
Climate change in Europe may boost transmission of Campylobacter, Salmonella, and non-cholera Vibrio species, according to a report today from the European Centre for Disease Prevention and Control (ECDC) on the effects of climate change on food- and waterborne disease. Researchers developed a relational database that included information from 741 peer-reviewed publications, reports, and other scientific sources. They then assessed how water and air temperature, seasonality, heavy rainfalls, precipitation, and temperature changes might affect various pathogens, anticipating increases in average temperatures, precipitation in some regions, and extreme weather. The investigators predicted the risk of campylobacteriosis to rise with mean weekly temperatures. They report that the link to temperature is even stronger with salmonellosis but that food-safety steps may help curb any increase in risk. They
also point out that Vibrio organisms undergo increased growth in coastal waters during hot summers. In contrast, they say that norovirus and Listeria show a much weaker link to climatic variables.
Mar 28 ECDC news release
Mar 28 ECDC report
Study: Whole-stool samples detect more pathogens in acute gastroenteritis
Whole-stool samples appear to be substantially better for detecting pathogens that cause acute gastroenteritis than rectal swabs, according to a study of emergency department patients published yesterday in the Journal of Infectious Diseases. US researchers studied 364 patients from three major medical centers in Connecticut, New York, and Oregon. Of those patients, 133 (37%) provided a whole-stool sample, 197 (54%) had a rectal swab, and 34 (9%) had both. Pathogens were detected in 25% of all patients but in 49% of those who provided a whole-stool specimen. Also, 9% of those with a whole-stool sample had more than one pathogen detected, compared with none in the rectal-swab group. The most commonly detected pathogens in whole-stool samples were norovirus (26%), rotavirus (18%), and Salmonella (5.3%); those percentages for rectal swabs were 7%, 3%, and 2%. The authors called the level of rotavirus
"surprising." An accompanying editorial states, "Although most persons presenting with acute diarrhea do not undergo stool studies, and only a very small proportion of routine stool cultures that are performed identify a pathogen, a substantial proportion of patients are treated with antimicrobials. It is imperative that data-driven differential diagnoses and improved diagnostics inform guidelines" for detecting and managing acute gastroenteritis.
Mar 27 J Infect Dis abstract
Mar 27 J Infect Dis editorial
Point-of-care flu microchip test performs well in trial
A point-of-care prototype microchip test performed better in detecting flu than other rapid tests and as well as common lab tests, according to a recent study in PLoS One. Boston University scientists tested a single-use microfluidic chip they developed that integrates solid-phase extraction and molecular amplification via reverse-transcription polymerase chain reaction (RT-PCR) to amplify the RNA of influenza type A viruses. After testing 146 specimens, they reported 96% sensitivity (95% confidence interval [CI], 89%-99%) and 100% specificity (95% CI, 95%-100%) compared with conventional RT-PCR. The positive predictive value was 100% (95% CI, 94%-100%) and the negative predictive value was 96% (95% CI, 88%-98%). In comparison, they found that direct fluorescent antigen (DFA) testing had 98% sensitivity and 96% specificity. The microchip test produces results in 3 hours or less. Lead author Catherine Klapperich, PhD, said
in a Boston University news release yesterday, "The new test represents a major improvement over viral culture in terms of turn-around time, over rapid immunoassay tests in terms of sensitivity (ability to detect the virus from minimal sample material), and over DFA and RT-PCR in terms of ease of use and portability."
Mar 22 PLoS One study
Mar 27 Boston University press release
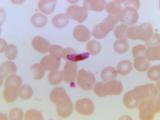
Older travelers may be more at risk of malaria death
Travelers over age 65 who visit malaria-endemic countries are more than 10 times as likely to die from the disease as are young adults, according to a BMJ study yesterday. UK researchers looked at 20 years of data on more than 25,000 UK patients. They found that most cases of malaria occurred in people of African heritage traveling to visit relatives, but that tourists not of African heritage were more than nine times as likely to die of the disease. Mortality increased steadily with age among all malaria patients, with a case-fatality rate (CFR) of 4.6% in those 65 and older and an adjusted odds ratio of death in that age-group of 10.7 (95% CI, 6.4-17.8), P < 0.001) compared with those 18 to 35 years old. CFR was 3.0% in tourists, compared with 0.32% in travelers of African heritage visiting friends and relatives. Those born in malaria-endemic African countries had a 0.4% CFR, compared with 2.4% for others. The team's
data also suggested that most patients who died presented late in the course of their illness. The authors emphasize that older travelers "are important groups to target in pre-travel advice."
Mar 27 BMJ abstract
Mar 28 BMJ news release