- US flu indicators showed more slight rises last week, though levels are still below baselines, the Centers for Disease Control and Prevention (CDC) said today in its latest update. The percentage of outpatient visits for flulike illnesses increased slightly, to 2.5%, but is still below the 2.9% baseline. Increases in hospitalizations were noted in six regions, but with levels stable in the Midwest, Northwest, and Northeast. Test positivity increased in the South and West, with influenza A making up 71.6% samples at clinical labs, mostly the 2009 H1N1 strain.
- Four countries reported more polio cases this week, including Pakistan, which reported another wild poliovirus type 1 (WPV1) case, bringing its total for the year to four, the Global Polio Eradication Initiative said in its latest weekly update. Three African nations reported more vaccine-derived cases, including the Democratic Republic of the Congo and Madagascar, with more circulating vaccine-derived poliovirus type 1 (cVDPV1) cases, and Kenya, with another circulating vaccine-derived poliovirus type 2 (cVDPV2) case.
- Highly pathogenic avian flu outbreaks struck more commercial turkey farms in four states—California, Minnesota, South Dakota, and Iowa—according to the latest notifications from the US Department of Agriculture (USDA) Animal and Plant Health Inspection Service (APHIS). Also, more outbreaks in backyard flocks were reported in Iowa, Oregon, and Minnesota. The events are part of an increase in avian flu activity that began in early October. In international developments, Bulgaria reported two H5N1 outbreaks on large poultry farms, Romania reported a detection involving backyard birds, and Mexico reported the virus in a healthy wild duck from a wetland in Jalisco state that was tested as part of surveillance, according to notifications from the World Organization for Animal Health (WOAH).
Quick takes: Slight US flu rise, more global polio, avian flu strikes more US poultry
SARS-CoV-2 Omicron variant more common, tied to more severe outcomes than flu, RSV

SARS-CoV-2 Omicron infections were more common and linked to more severe outcomes than influenza and respiratory syncytial virus (RSV) in emergency department (ED) patients in Sweden, especially among those unvaccinated against COVID-19.
The findings were published yesterday in Clinical Infectious Diseases.
Karolinska Institutet researchers assessed rates of 30-day all-cause death, hospitalization, and intensive care unit (ICU) admission of adults seen in six EDs in Stockholm County for Omicron, flu, or RSV infection in 2021-2022 and 2015-2019. Of 6,385 patients in 2021-2022, 76% were infected with Omicron, 17% had flu, and 7% had RSV.
In total, 22.1% of Omicron patients were unvaccinated against COVID-19 before their ED visit, while 75% had received at least two doses.
Lower odds of death after COVID vaccination
Thirty-day death rates were 7.9% in the Omicron group, 2.5% in flu patients, and 6.0% in the RSV group. Omicron patients' adjusted death odds ratio (OR) was 2.36 compared with flu and 1.42 compared with RSV. Stronger links were seen in unvaccinated Omicron patients relative to flu (OR, 5.51) and RSV (OR, 3.29).
Death rates at 30 days were 15% among Omicron patients aged 75 years or older, compared with 8% in the 2021-2022 flu group, 12% in the 2021-2022 RSV cohort, 7% among 5,709 prepandemic flu patients, and 9% among 955 prepandemic RSV patients. Among Omicron patients who received at least two COVID-19 vaccine doses, the OR for death was 2.00 compared with flu and 1.20 compared with RSV.
This underscores the need for public health strategies for managing and mitigating the impact of Omicron and other viral respiratory infections, with continued assessments of their comparative severity.
Ninety-day mortality was 11% among Omicron patients, 3.7% in 2021-2022 flu patients, 8.7% in 2021-2022 RSV patients, 5.1% in the prepandemic flu group, and 9.6% in prepandemic RSV patients.
In 2021-2022, 30-day mortality was 2.6% for influenza A patients; none of the 17 influenza B patients died. From 2015 to 2019, 30-day mortality was 3.2% in influenza A patients and 3.8% in influenza B patients.
"This underscores the need for public health strategies for managing and mitigating the impact of Omicron and other viral respiratory infections, with continued assessments of their comparative severity," the authors wrote.
Pfizer and BioNTech report positive findings for COVID-flu mRNA combo vaccine
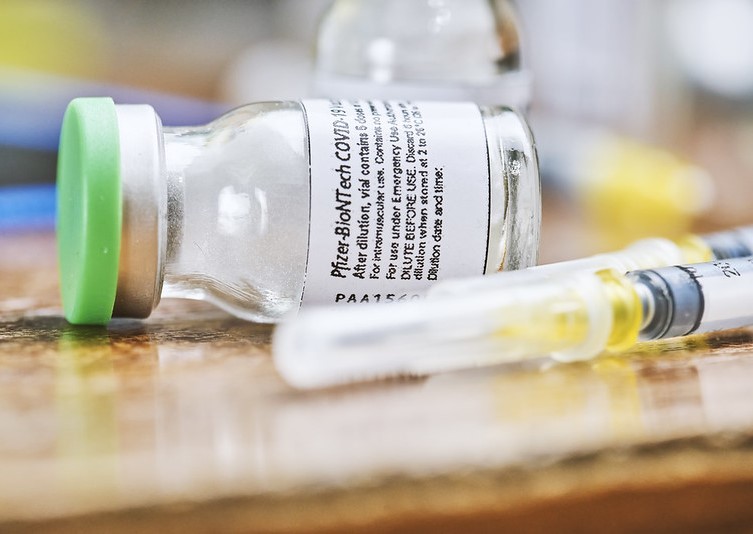
Moderna and BioNTech yesterday announced promising findings for their phase 1/2 trial of an mRNA vaccine that targets both COVID and flu.
Scientists tested different combo vaccine candidates in healthy adults ages 18 to 64 against a licensed flu vaccine and the companies' earlier bivalent (two-strain) COVID vaccine, with both vaccines given at the same visit. Lead formulations of the combo vaccines prompted robust immune responses against influenza A, influenza B, and SARS-CoV-2, the virus that causes COVID-19.
The safety results for the combo vaccines were similar to the vaccine against COVID.
Based on the findings, the companies said they would advance the lead formulations to a phase 3 trial in the months ahead. The Food and Drug Administration (FDA) has given the company fast-track designation for the new vaccine.
Annaliesa Anderson, PhD, Pfizer’s senior vice president and head of vaccine development, said in a statement that the companies are encouraged by the early trial results, which will appear in a peer-reviewed journal soon. “This vaccine has the potential to lessen the impact of two respiratory diseases with a single injection and may simplify immunization practices for providers, patients, and healthcare systems all over the world,” she said.
Earlier this month, Moderna reported promising findings from an early clinical trial of its mRNA combo vaccine against flu and COVID.











