Our weekly wrap-up of antimicrobial stewardship & antimicrobial resistance scans
NICU program associated with lower sepsis, better antibiotic prescribing
The neonatal intensive care unit (NICU) at Yale University School of Medicine significantly reduced its cases of late-onset sepsis, a leading cause of death among preterm infants, by implementing guidelines designed to eliminate antibiotic overuse, according to a new study in Infection Control & Hospital Epidemiology, the journal of the Society for Healthcare Epidemiology of America (SHEA).
A team of experts developed the antibiotic stewardship program, which consists of clinical guidelines published to the hospital intranet to curtail provider-to-provider variability in prescriptions and to educate NICU staff. The NICU antibiotic stewardship guidelines reduced variability in treating common infections, improving clinical adherence to best practices.
Using electronic medical records, the stewardship team reviewed a daily report of all prescribed antimicrobials and provided timely prescriber oversight and feedback.
The researchers found that healthcare-associated infections decreased after program implementation, including evaluations for late-onset sepsis, with an average reduction of 2.65 late-onset sepsis evaluations per year per provider. Overall, the rate of late-onset evaluations per 100 days dropped from 21.2 to 8.4. The data also showed that physicians followed antibiotic prescribing guidelines 98.75% of the time, and no infants with clinical infections developed a recurrent infection after 7 days of discontinuing antibiotic treatment.
"So few antimicrobial stewardship programs provide NICU-specific guidelines to cut down on unnecessary prescription practices," said study author Matthew Bizzarro, MD, in a SHEA news release. "Our use of an electronic medical record-generated daily report, with additional information on the rationale behind each prescription event was somewhat novel and incredibly useful in providing timely feedback and review of prescriber practices."
Jul 26 Infect Control Hosp Epidemiol abstract
Jul 27 SHEA news release
Vaccine candidate for recurrent MDR UTIs fast-tracked by FDA
Originally published by CIDRAP News Jul 27
Sequoia Sciences announced yesterday that it has received fast-track designation from the US Food and Drug Administration (FDA) for its investigational vaccine designed to treat recurrent urinary tract infections (UTIs) caused by multidrug-resistant (MDR) bacteria. Fast-track designation expedites the development and review of the vaccine through the US regulatory process.
Sequoia's vaccine is designed to produce an immune response preventing bacteria from colonizing the urinary tract, and it recently completed its first clinical trial in women. Among the 67 women enrolled in the study, 30 of whom had a 2-year history of recurrent UTI, the vaccine was well-tolerated and generated a strong immune response, the company said in a news release.
Based on these results, Sequoia has begun additional studies, including evaluating the vaccine in patients requiring antibiotics of last resort. In granting fast-track status, the FDA acknowledges that recurrent UTI caused by MDR bacteria is a serious condition for which there is an unmet medical need, Sequoia said.
"If approved, the vaccine could change the standard of care for recurrent UTI," said Gary Eldridge, president and CEO, Sequoia Sciences. "Since UTI[s] are a primary source of sepsis, decreasing recurrent UTI may ultimately drive down rates of hospitalization, sepsis, and associated in-hospital mortality."
Currently, patients who have recurrent UTI frequently take daily antibiotics for 1 to 4 months or even longer, which can lead to drug resistance, according to the release. Each year, about 3 million patients in the United States and 10 million in North America, Europe, and Japan experience recurrent UTI, about half of which is caused by antibiotic-resistant bacteria.
Jul 26 Sequoia Sciences news release
Group develops roadmap for MDR gonorrhea
Originally published by CIDRAP News Jul 27
Yesterday an international group of experts published a research and development roadmap for the discovery of new drugs for MDR gonorrhea, part of efforts by the Global Antibiotic Research and Development Partnership (GARDP), which was launched by the World Health Organization and Drugs for Neglected Disease initiative last year.
The roadmap, published as a commentary in PLoS Medicine, lays out a 7-year plan for health officials and includes four main components and a target product profile (TPP) for new medicines.
The number of gonorrhea cases has risen in many areas across the globe, an increasing proportion of which are MDR. The choice of treatment options for gonorrhea is very limited, and resistance has even been reported to extended-spectrum cephalosporins, the mainstay of current first-line therapy. Also, only three new chemical entities are in different stages of clinical development for treatment of gonorrhea, the experts report.
The plan's key components are: (1) accelerate development of a new molecule to treat the disease, (2) evaluate the potential of existing antibiotics and combinations, (3) explore co-packaging and development of fixed-dose combinations, and (4) support the development of simplified treatment guidelines and foster conservation.
The TPP includes "ideal" and "acceptable" criteria for such factors as indication, tolerability, cost, stability, and dosing schedule for new gonorrhea drugs.
The authors write, "Over the next 7 years, this research and development proposal includes the following: exploring the introduction of a new clinical entity against gonorrhea; the identification of existing, suitable partner drugs; the recovery of previously abandoned, out-of-favor, and withdrawn antibiotics; and the development of simplified treatment guidelines for the empiric management of sexually transmitted infections."
Jul 26 PLoS Med commentary
GARDP TPP
Analysis finds follow-up blood cultures unnecessary for bacteremia
Originally published by CIDRAP News Jul 27
An analysis of 383 bacteremia cases by University of Texas scientists has determined that follow-up blood cultures for gram-negative bacteremia are unnecessary and contribute to increased healthcare costs, longer hospital stays, unnecessary consultations, and inappropriate use of antibiotics.
The researchers, reporting in Clinical Infectious Diseases yesterday, analyzed data on 383 bacteremia patients who had at least one follow-up blood culture (FUBC). They gleaned information on presumed source of disease, antibiotic status at the time of FUBC, antibiotic susceptibility, presence of fever, comorbidities, need for intensive care, and mortality.
They found that antibiotic use did not affect the rate of positivity of FUBC, unless bacteria were not sensitive to the empiric antibiotic. Fever on the day of FUBC was associated with higher rates of positive FUBC for gram-positive cocci but not gram-negative bacilli (GNB). Mortality and care in the intensive care unit were also not associated with a positive FUBC.
The authors conclude, "FUBC added little value in the management of GNB bacteremia. Unrestrained use of blood cultures has serious implications for patients, including increased healthcare costs, longer hospital stays, unnecessary consultations, and inappropriate use of antibiotics."
Jul 26 Clin Infect Dis abstract
Scottish data platform helps inform Infection control, stewardship
Originally published by CIDRAP News Jul 27
A new paper in the Journal of Antimicrobial Chemotherapy describes efforts in Scotland to use patient data to better understand the epidemiology of infectious disease and inform and evaluate antimicrobial stewardship programs.
The objective of the Infection Intelligence Platform (IIP), which is led by the Scottish Antimicrobial Prescribing Group (SAPG) and supported by National Health Services Scotland (NHS), is to create a national infection informatics resource for infection control and stewardship clinicians. The program is focused on three objectives: Developing a technical platform to link the various NHS patient datasets to enhance surveillance capability; establishing a governance process that ensures the data is secure and accessible; and using the data to generate new evidence to guide clinical practice.
The authors report that in the build-out and test phase of the IIP, they have improved data security, created "simplified views" of the complex datasets, and embedded statistical programs to enhance capability. These developments have enabled researchers to conduct studies using the datasets. These studies have measured the intended and unintended effects of antimicrobial stewardship and infection management intervention and examined infection risk factors and clinical outcomes.
Findings from the studies have been disseminated to clinicians through the IIP website, regular newsletters, and presentations at international meetings, and the authors say the evidence is already shaping clinical practice.
"We are part way along our IIP journey and have begun to increase our responsiveness to address important clinical questions that could be answered through a data linkage approach," the authors write. "We hope our shared experience will inform and encourage others to embark upon this journey and catalyse opportunities for global collaboration."
Jul 10 J Antimicrob Chemother paper
New class of antibiotics shows promise against MDR bacteria, plague
Originally published by CIDRAP News Jul 26
An experimental drug that belongs to a new class of antibiotics showed promise in lab tests against multidrug-resistant (MDR) gram-negative bacteria, and was protective against the bacterium that causes plague in mice, according to a study yesterday in mBio.
Researchers from Lille, France, and Duke University demonstrated that LPC-069, a drug in the class called LpxC inhibitors for their ability to inhibit LpxC, a critical gram-negative bacterial enzyme, was effective in cell-culture tests against a dozen pathogenic bacterial taxa. The bacteria were isolated from hospitalized patients in Lille and included MDR strains such as extended-spectrum beta-lactamase–producing and carbapenemase-producing Enterobacteriaceae, Pseudomonas aeruginosa, and Acinetobacter baumannii.
The new drug also protected mice from Yersinia pestis, the bacterium that causes plague. A similar drug (called LPC-058) also was effective against Y pestis, but it led to side effects such as diarrhea, accumulation of white blood cells, and, at the highest doses, liver toxicity. LPC-069, in contrast, caused no serious side effects at any of the doses tested.
"Our study shows that LpxC is a viable target, and we can dose the compound (LPC-069) at very high levels without noticeable toxicity," said Pei Zhou, PhD, of Duke, in a press release from the American Society for Microbiology (ASM), which publishes mBio.
LpxC is one of the six essential enzymes in the lipid A pathway in gram-negative bacteria, and Zhou and his colleagues suspect that other essential lipid A enzymes might also be valuable targets for antibiotic treatment. The team next plans to test the efficacy of LPC-069 in animals against a range of gram-negative pathogens.
Jul 25 mBio study
Jul 25 ASM news release
Triple-drug combo to battle superbugs carrying MCR-1 and NDM-5
Originally published by CIDRAP News Jul 26
A study to pinpoint a drug combination to treat bacteria that carry two of the most worrisome antibiotic resistance genes—MCR-1 and NDM-5—found a triple-combination cocktail of antibiotics helped eradicate Escherichia coli that contained both genes.
An E coli isolate containing both resistance genes was recently isolated in a patient from New Jersey, the first such detection in the United States, who had a history of prostate cancer and had recurrent urinary tract infections, raising fears that hospitals may soon be facing large outbreaks of Enterobacteriaceae that produce MCR-1 and New Delhi metallo-beta-lactamase (NDM). Researchers published their findings on a possible treatment in yesterday in mBio.
They assessed bacterial killing of 15 different antibiotics approved by the Food and Drug Administration (FDA), alone and in combination with polymyxin B. The three-drug combination of polymyxin B, aztreonam, and amikacin completely eradicated and suppressed the E coli that harbored both genes, which the researchers said would help clinicians prepare for future cases involving the same type of organism.
Jul 25 mBio study
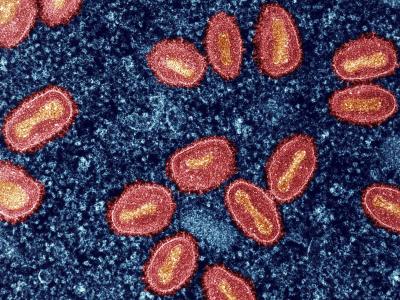
Recent hospital MRSA drop largely due to soft-tissue infections
Originally published by CIDRAP News Jul 26
US investigators reported today that the decline for hospitalizations for methicillin-resistant Staphylococcus aureus (MRSA) in recent years was primarily due to declines in skin and other soft-tissue infections, and invasive MRSA-related hospitalizations remained largely unchanged.
The researchers, reporting in Clinical Infectious Diseases, calculated rates of MRSA-related hospitalizations from 2010 to 2014 using the National Inpatient Survey (NIS), which includes millions of patient records. The number of MRSA-related hospitalizations decreased 15.8% during that period, from 423,242 to 356,315, and the rate of MRSA-related hospitalizations decreased from 11.31 to 10.08 per 1,000 hospitalizations.
The decline in MRSA-related hospitalizations was primarily attributable to a decrease in unspecified MRSA-related infections which fell from 8.32 to 7.17 per 1,000 hospitalizations. MRSA-related pneumonia infections decreased as well, though only between 2013 and 2014, and accounted for only 13% of the overall decrease, falling from 1.54 to 1.38 per 1,000 hospitalizations. The rate of MRSA-related septicemia, though, increased slightly, from 1.45 to 1.53 per 1,000 hospitalizations.
The most frequent primary diagnoses associated with "other" MRSA-related infections were cellulitis and abscess infections. Rates of MRSA-related skin and other soft-tissue infections decreased 29%, from 3.8 to 3.0 per 1,000 hospitalizations. Rates for other common primary diagnoses associated with unspecified MRSA-related infections did not change much during the study period.
The authors conclude, "The decrease in rates of noninvasive MRSA hospitalizations may be attributable to a combination of efforts to combat this public health crisis. However, because the decrease was largely confined to community-associated infections, these changes may instead reflect the natural waning of an epidemic."
Jul 26 Clin Infect Dis report
CARB-X awards $17.6 million to fund new antibiotic development
Originally published by CIDRAP News Jul 25
CARB-X, the international public-private initiative to stimulate new antimicrobial development, today announced the winners of its second round of funding.
The seven projects to receive funding from CARB-X (the Combating Antibiotic Resistant Bacteria Biopharmaceutical Accelerator) include five potential new class antibiotics for gram-negative bacteria, a potential new treatment for drug-resistant gonorrhea, and a new molecule targeting a superbug that causes infections in cystic fibrosis patients. The companies will share $17.6 million to speed pre-clinical development of their products. The money will also fund a phase 1 clinical trial of a new oral broad-spectrum antibiotic.
Two of the companies are based in the United States. The others are in the United Kingdom, Ireland, France, and India.
"We are looking to support the best potential new treatments and diagnostics across the world," CARB-X Executive Director Kevin Outterson, JD, said in a press release. "We are especially pleased that today's awards mean we are now supporting scientists in six countries."
CARB-X is funded by the Biomedical Advanced Research and Development Authority (BARDA) and the Wellcome Trust, a global charitable foundation based in London, with additional support from the National Institute of Allergy and Infectious Diseases (NIAID). It's the world's largest public-private partnership devoted to preclinical antibacterial research and development.
In its first round of funding, announced Mar 30, CARB-X awarded $24 million to 11 biotech companies. The initiative has pledged to commit $450 million over 5 years to spur new antibiotic research and development.
Jul 25 CARB-X press release
Global study notes higher improper prescribing with antibacterials
Originally published by CIDRAP News Jul 25
An analysis published late last week involving prescribing data from 53 countries found higher rates of improper antibacterial prescribing compared with antifungal prescribing.
Writing in the Journal of Antimicrobial Chemotherapy, Belgian scientists reported data on 48,565 prescriptions (43,513 [90%] for antibacterials and 2,062 [4%] for antifungals for systemic use) given to 34,731 patients in early 2015. The reasons for prescribing (77.7% vs 71.8%) and stop/review dates (38.3% vs 31.9%) were found more often in notes for antibacterials than for antifungals.
The team found that antibacterials were prescribed according to local guidance only 57.0% of the time, compared with 71.0% for antifungals.
The authors conclude, "All of the quality indicators in this study can be used to improve the quality of antimicrobial prescribing. For example, the proportion of the oral mode of administration can be increased among antibacterials with excellent bioavailability since oral therapy is easy to give and cheaper than intravenous therapy. . . . Another example is issuing antimicrobials by the pharmacist only if the reason for the prescription is documented in the patient's notes."
Jul 21 J Antimicrob Chemother study
Study estimates $800,000 cost of an NDM-1 hospital outbreak
Originally published by CIDRAP News Jul 24
A new study in Emerging Infectious Diseases describes the physical and financial burden of a nosocomial outbreak caused by New Delhi metallo (NDM) beta-lactamase–containing Klebsiella pneumoniae.
The 2015 outbreak, which occurred at a tertiary teaching hospital in the Netherlands from Oct 1 to Dec 30, began when NDM-1–producing extended-spectrum beta lactamase (ESBL)-positive K pneumoniae bacteria were cultured and isolated from a patient in the surgical ward. Following that discovery, screening cultures of long-term admitted surgical patients revealed 2 more patients with NDM-producing K pneumoniae, and contact tracing and weekly screening rounds of all hospital patients revealed additional NDM carriers. A total of 29 patients were affected.
An assessment of outbreak-related expenses estimated the total costs of the 3-month outbreak at $804,263, corresponding to a cost of $27,770 per patient. The loss of revenue was mainly attributed to closure of beds during the outbreak. Other cost drivers were diagnostic tests and personnel time spent by laboratory employees and infection prevention experts.
"As shown in this study, the expansion of multidrug-resistant, gram-negative bacteria is of great concern; these bacteria both threaten patient safety and increase healthcare costs," the study authors write. "The intensive outbreak control measures of the hospital were costly and inconvenient for patients and staff."
The authors say that in countries where NDM-positive K pneumoniae is not endemic, early detection of colonized patients and adequate infection control strategies will be important factors in minimizing the spread of the multidrug-resistant bacteria.
Jul 21 Emerg Infect Dis dispatch
ASP associated with reduced mortality in patients treated with vancomycin
Originally published by CIDRAP News Jul 24
Mortality in older patients treated with vancomycin decreased by 7.1% after an antimicrobial stewardship program (ASP) was implemented, researchers at a Veteran Affairs hospital report in the American Journal of Infection Control.
In the retrospective quasi-experimental study, researchers at the Veterans Affairs Western New York Healthcare System in Buffalo, New York, aimed to evaluate the impact of an ASP on 30-day mortality rates in patients treated with intravenous (IV) vancomycin, which is the drug of choice for infections caused by MRSA but has been associated with nephrotoxicity. ASP interventions consisted of prospective audit and feedback, including appropriate antibiotic selection and dosing, microbiology, and duration of treatment. A secondary outcome was to determine risk factors for mortality associated with vancomycin.
Overall, 453 patients were treated with a minimum of 48 hours of IV vancomycin therapy during the study period—226 in the pre-ASP period (Oct 1, 2006 through Jul 31, 2008) and 227 during the ASP period (Aug 1, 2011 through Jul 31, 2014). Clinicians using the ASP made on average about four vancomycin recommendations per patient. Deaths occurred in 56 patients (12.4%), with 36 (64.3%) occurring during the pre-ASP period and 20 during the ASP period (P =.02). Patients in the ASP group also had less nephrotoxicity than those in the pre-ASP group (17 vs 31 patients).
Increased mortality was associated with pre-ASP years (odds ratio [OR]. 2.17), older age (OR, 1.08), nephroxicity (OR, 3.24), and hypotension (OR, 3.28). Treatment in the intensive care unit was also associated with higher mortality.
"Our prospective audit and feedback system was associated with improved mortality in an older population with a mean age of 68 years," the study authors write. "The process of comprehensive patient review, including culture data and imaging and close monitoring of any changes in renal function, may be necessary for the elderly patient beyond computerized support software to achieve improved rates of morality."
Jul 21 Am J Infect Control study
US data show increases in Campylobacter cases, outbreaks, resistance
Originally published by CIDRAP News Jul 24
The number of US Campylobacter outbreaks has doubled in recent years, and isolates have proved increasingly antibiotic resistant, according to a study last week in Clinical Infectious Diseases.
The researchers analyzed data on more than 300,000 Campylobacter infections from 2004 through 2012. The average annual incidence rate (IR) was 11.4 cases per 100,000 people, with the rate varying from 3.1 to 47.6 by state. IRs among preschool children were double the overall rate. Overall IRs increased 21%—from 10.5/100,000 in 2004-06 to 12.7/100,000 in 2010-12.
Over the study period, 347 Campylobacter outbreaks were reported. The annual median number of outbreaks doubled, from 28 in 2004-06 to 56 in 2010-12.
Antimicrobial susceptibility testing of isolates from 4,793 domestic and 1,070 travel-associated cases revealed that ciprofloxacin resistance increased among domestic infections from 12.8% in 2004-09 to 16.1% in 2010-12, a 26% increase.
The authors conclude, "These data provide baseline rates for monitoring change now that campylobacteriosis is a nationally notifiable disease," which occurred in 2015.
Jul 20 Clin Infect Dis study